Background
One of the most prominent barriers to virtual care are the antiquated state licensure laws that limit the ability of health care providers to see patients across state lines. State lines create artificial barriers to the delivery of care – complicating access for patients and creating additional burden on clinicians. These lines sometimes split major urban areas and hamper the ability of telemedicine providers to fill in gaps in the delivery system and provide high value care directly to consumers in rural or underserved areas. Current efforts to expand interstate licensure have been insufficient to meet the needs of patients and the clinicians seeking to better serve them.

Health care professionals are prohibited from treating patients in states where they are not licensed, but the state-by-state licensing processes are burdensome and expensive. Uniform national standards across clinical practice areas are in place, but there is wide variation in state licensing processes. In the case of physician licensure, all states require postgraduate training, proof of successful completion of all three steps of the U.S. Medical Licensing Examination, and training verification forms. However, some states add additional unique requirements for medical licensure such as background checks, fingerprinting, completing continuing medical education requirements, providing additional documents such as birth certificates, or even character witnesses. Another barrier is the expense. Licenses in a single state can cost upwards of $1,000, and application fees on top of licensing fees can add up.
Impact of COVID-19 on Licensure
COVID-19 has exposed the barriers posed by the fragmentation of state practice act laws and regulations. The ability for licensed, credentialed health care professionals to provide patient care across state lines via telehealth during the pandemic helped maintain continuity of care, promoted patient choice, helped address workforce shortages, and improved care coordination. Telehealth also helped improve patient access to primary and specialty care, boosted patient and caregiver engagement, reduced missed appointments, and improved post-operative care.
At the outset of the pandemic, the federal government took action at the start of the pandemic to address care across state lines. CMS temporarily waived requirements that out-of-state Medicare practitioners be licensed in the state where they are providing services when they are licensed in another state. CMS also released guidance stating that state Medicaid agencies could use Section 1135 waiver authority to permit providers located out of state to provide care to another state’s Medicaid enrollee impacted by the COVID-19 emergency.
Governors across the country also took action to address licensure laws to ensure access to care. These licensure flexibilities provided health care practitioners more flexibility to treat patients in other states when there were pressing needs or specialized expertise not available where they lived. Our experience during the pandemic has provided an unprecedented opportunity for patients, providers, and policymakers to explore the impact of cross-state care. We have seen it benefit the delivery of health care in many ways, but most notably through new avenues for patient access to care.
As state emergency declarations enacted at the start of COVID-19, including licensure and telehealth flexibilities, began to expire, providers had to go back to cumbersome and expensive state-by-state licensing requirements if they wanted to continue to help patients in other states. Without a glidepath or permanent policy measures to adjust to these changes, patients have to either travel long distances to see a provider in person or cancel appointments, which creates a barrier to accessing convenient care and to continuity of care.
Uniform Telehealth Act
In 2022, the Uniform Law Commission made available to states model legislation called the Uniform Telehealth Act, which aims to give states the clear guidance and framework they need to facilitate the delivery of services via telehealth consistent with the standard of care of the state in which the patient is located. In recent years, improvements in telecommunication technologies have transformed the delivery of health care. The arrival of the COVID-19 pandemic greatly expanded patient demand for telehealth services. To meet patient needs, many states chose to modify licensure and other requirements that served as barriers to the delivery of telehealth services. Today, many states are re-examining laws related to telehealth, often with an eye toward expanding access to care while maintaining protections for patients.
The Uniform Telehealth Act has two broad goals. The first is to make clear that, as a general matter, health care services may be provided through telehealth, if doing so is consistent with applicable professional practice standards and the practitioner’s scope of practice, as defined by the state in which the patient is located. The Telehealth Act’s second goal is to establish a registration system for practitioners who hold licenses in other states. This act permits a registered practitioner to provide telehealth services to patients located in the state adopting the act. The ULC hopes the Act will give states the clear guidance and framework they need to implement effective telehealth services, as well as open borders so that more practitioners are able to assist patients that might otherwise have limited access to health care.
Alliance Advocacy Highlights
The Alliance has championed a number of initiatives to address this issue and advocate for more flexibility to provide care via telehealth across state lines. See below for our advocacy on this issue. Please contact Rikki Cheung at rikki.cheung@connectwithcare.org if you have any questions about this topic.
CONGRESS
Legislation
- TELEmedicine for MEDicare (TELE-MED) Act – First introduced in 2013 (H.R. 3077) by Reps. Nunes (R- CA) and Pallone (D-NJ) and later reintroduced in 2015 by Reps. Nunes and Pallone and Sens. Hirono (D-HI) and Ernst (R- IA) (H.R. 3081/S. 1778). This bill would have permitted certain Medicare providers to provide telemedicine services to a Medicare beneficiary who is in a different state from the one in which the provider is licensed or authorized to provide health care services. The licensing or authorizing state has jurisdiction to enforce its licensure or other legal authorization requirements with regard to such a provision of service.
- Temporary Reciprocity to Ensure Access to Treatment (TREAT) Act – First introduced in 2020 by Reps. Latta (R-OH) and Dingell (D-MI) and Sens. Murphy (D-CT) and Blunt (R-MO) (H.R. 8283/S. 4421), and later reintroduced by same co-sponsors in 2021 (H.R. 708/S. 168). This bill would temporarily authorize the interstate provision of in person and telehealth services. This authorization would apply during, and for at least 180 days after, the COVID 19 public health emergency. Subject to scope of practice and other requirements, a health care professional may provide health services in any U.S. jurisdiction based on that individual’s authorization to practice in any one state or territory. The bill also provides certain related powers to health care professional regulatory bodies, such as medical boards. Specifically, regulatory bodies may investigate and take disciplinary actions against a professional who provides services pursuant to this bill to a patient in that body’s jurisdiction.
- Accelerating Kids’ Access to Care Act – Introduced by Sens. Grassley (R-IA) and Bennet (D-CO) and Reps. Clark (D-MA) and Herrera Beutler (R-WA) in May 2021 (S. 1544/H.R. 3089). This bill would streamline enrollment under the Medicaid program of certain providers across state lines. The bill requires state Medicaid programs to establish a process through which qualifying out-of-state providers may enroll as participating providers without undergoing additional screening requirements.
- Compacts, Access and Responsible Expansion (CARE) for Mental Health Professionals Act – Introduced by Rep. Neguse (D-CO) in November 2021 (H.R. 6076) and Sen. King (I-ME) in April 2022 (S. 4058). This bill would reform medical licensure to expand interstate access to mental health resources. The bill would require HHS to establish the Mental Health Licensure Portability Program to award grants to eligible entities for projects to: incentivize counselors to practice in states that have entered into interstate compacts for the purpose of expanding the workforce of credentialed mental health professionals; and Develop, operate or maintain interstate compact commissions authorized to effectuate the provisions of interstate compacts entered into by such states.
- Telehealth Treatment and Technology (3T) Act – Introduced by Reps. Cawthorn (R-NC) and Gosar (R-AZ) in March 2022 (H.R. 7097). This bill would facilitate the provision of telehealth services through interstate recognition of health care professionals’ licenses.
- States Handling Access to Reciprocity for Employment (SHARE) Act – Introduced by Reps. Mann (R-KS), Neguse (D-CO), and 18 cosponsors in March 2023 (H.R. 1310). This bill would authorize the use of FBI criminal history record information for administration of interstate compacts. Specifically, the FBI must furnish or otherwise make available to a state licensing authority, through an agreement with a state law enforcement agency or state identification bureau, criminal history record information to the extent required by an interstate compact, for purposes of conducting a criminal history background check of individuals seeking a license or privilege to practice an occupation or profession in a compact member state.
Other Notable Action
Senate Finance Committee: Medicaid Interstate Licensure Provision Included in the Youth Mental Health Discussion Draft (6/15/22) – Senate Finance Committee Chair Wyden (D-OR), Ranking Member Crapo (R-ID), Senator Carper (D-DE) and Senator Cassidy (R-LA) released the second draft section of the Committee’s mental health package. This portion focuses on youth mental health care policies as part of the Committee’s ongoing work to improve mental health. The draft includes language that would simplify the process for eligible out-of-state providers to enroll as a participating provider in state Medicaid or CHIP plans without additional screening requirements, among other provisions.
Inside Telehealth: Senate Finance Telehealth Draft Requires CMS Continue to Embrace Interstate Compacts (6/3/22) – In the recently released Senate Finance’s draft telehealth-mental health bill, the bill provides a vague paragraph on interstate licensing. A Senate staffer clarified the language on interstate licensing in the Senate Finance’s draft telehealth-mental health bill. The staffer clarified that Section 8 of bill requires that CMS regularly update its current coverage guidance to make it clear Medicare covers tele-mental health services when a practitioner participates in a state that is part of an interstate licensure compact and the beneficiary is also located in a state that recognizes the compact.
ADMINISTRATION
HRSA Office for the Advancement of Telehealth: Interstate Licensure Resources (May 2023) – The HRSA Office for the Advancement of Telehealth released new interstate licensure resources. These resources include the latest guidance on how to practice telehealth across state lines legally and ethically while encouraging the uptake of licensure models that increase access to health care. The four resources include:
- Getting started with licensure: Learn about licensing and the role of states and the federal government.
- Licensing across state lines: Read how to deliver health care services, including through telehealth, across state lines.
- Licensure compacts: Find out more about compacts between states that make it easier for health care providers to deliver telehealth care for a range of specialties.
- Licensure for behavioral health: Explore resources specifically for behavioral health professionals who are subject to state licensure law and regulations, including for telehealth services.
White House: In State of the Union, President Biden to Outline Vision to Advance Progress on Unity Agenda in Year Ahead (February 2023) – In advance of President Biden’s 2023 State of the Union address, the White House released a four-part Unity Agenda focused on areas where members of both parties can come together and make additional progress for the American people. Most notably, the agenda highlights work to expand access to telehealth by tripling resources for HHS to promote interstate license reciprocity for delivery of mental health services across state lines. For additional coverage, see Inside Telehealth.
Strategy to Address the National Mental Health Crisis (March 2022) – On March 1, 2022, President Biden announced his strategy to address the national mental health crisis during his first State of the Union. This strategy will strengthen system capacity, connect more Americans to care, and create a continuum of support to transform our health and social services infrastructure to address mental health holistically and equitably. As part of this strategy, President Biden included a goal to expand access to tele- and virtual mental health care options. This includes that the Administration will work with Congress to ensure coverage of tele-behavioral health across health plans, and support appropriate delivery of telemedicine across state lines, to maintain continuity of access
Inside Telehealth: Biden Administration Pursues Interstate Licensing for Behavioral Practitioners (May 2022) – The White House is exploring multiple pathways to address barriers to interstate licensing for mental health practitioners, which includes plans the Administration could enact on its own and others that would be in conjunction with Congress. The Administration is considering removing interstate licensing barriers for decentralized clinical trials, among other strategies. Although interstate licensing has recently caught the attention of federal legislators with the rapid expansion of telehealth, Congress is limited in what it can do to remove licensing barriers for practitioners because state licensing boards have primary jurisdiction over the issue. Increased interstate licensing would make specialized care more accessible to a wider population, like behavioral health care, especially for patients in rural and underserved areas.
Journal of Medical Regulation: Increasing Access to a Diverse Mental Health Workforce Through Emergency Reciprocity Licensure (4/6/23) – New Jersey’s COVID-19 Temporary Emergency Reciprocity Licensure Program provided temporary licenses to more than 31,000 out-of-state health care practitioners, over a quarter of whom were mental health providers. As the need for mental health care accelerated during the pandemic, especially among health disparity populations, expanding mental health provider pools may be a critical tool to increase access to care. In January 2021, researchers at Rutgers surveyed New Jersey’s temporary licensees, analyzing over 4,500 mental health provider responses to examine the impact of the temporary licensure program on access to mental health care overall and on enhancing a diverse mental health workforce. Over 3,700 respondents used their temporary license to provide mental health care to New Jersey patients. Findings suggest that temporary out-of-state mental health providers helped enhance mental health care continuity and access.
Alma: Expanding Care with Teletherapy (3/27/23) – Alma, a digital health company, surveyed over 200 therapists and found that nearly nine in 10 of its therapists want to be able to provide care across the country if their license enabled them to provide care nationwide. The survey also found 67 percent of therapists have already pursued or are considering pursuing licenses in one or more additional states. Of these therapists, about half wanted to maintain relationships with current clients that moved or have moved across state lines. In the last year, 70 percent of therapists had to stop working with a client because they moved, even if they were solely seeing the client virtually.
Cicero Institute: Few Disciplinary Issues with Out-of-State Telehealth (3/22/23) – This report reviews the states of Florida and Idaho’s approach to out-of-state clinicians providing care to residents of those states via telehealth, and found that there were no cases that resulted in disciplinary action for an out-of-state provider offering services via telehealth in these states. Additionally, there was a substantial and growing number of providers interested in providing telehealth across state lines. Despite the attention telehealth has received during the pandemic, few states have implemented robust laws allowing out-of-state clinicians to provide care in their state. As policymakers review their current laws to best help their state be ready for another pandemic, or to improve access to affordable care, Florida and Idaho offer some lessons on providing telehealth care across state lines for them to consider. Key findings from the study include:
- In the first two and a half years that Florida has allowed out-of-state telehealth registrations, there have been no cases that have resulted in discipline for a provider offering services to Florida patients.
- Data from the Idaho Division of Occupational & Professional Licenses show that during the pandemic, no final disciplinary action was taken against a provider for care delivered over telehealth.
- Based on complaints data, there have been few complaints, and none have resulted in disciplinary action. These early results question the concern that there will be substantial disciplinary concerns with across-state-line telehealth.
JAMA Health Forum: Receipt of Out-of-State Telemedicine Visits Among Medicare Beneficiaries During the COVID-19 Pandemic (9/16/22) – This study focused on how out-of-state telemedicine was used during the COVID-19 pandemic, examining telemedicine visits in the first half of 2021 (Jan – June) among patients with traditional Medicare coverage. Key findings from the study include:
- Of the 8,392,092 patients with a telehealth visit, 422,547 patients (5 percent) had one or more out-of-state telemedicine visits.
- In 62.6 percent of all out-of-state visits, a prior in-person visit occurred between the same patient and clinician between March 2019 and the visit, showing that out-of-state telemedicine visits were largely used for continuity of care purposes with an existing provider-patient relationship.
- These visits were most common among those who lived near a border (57.2 percent of out-of-state visits).
- Visits were largely for primary care and mental health treatment (64.3 percent of out-of-state visits).
- People in rural communities were more likely to receive out-of-state telemedicine care (33.8 percent vs 21 percent).
- There was high out-of-state telemedicine use for cancer care (9.8 percent of all telemedicine visits for cancer care).
Health Affairs: Interstate Telehealth Use By Medicare Beneficiaries Before And After COVID-19 Licensure Waivers, 2017–2020 (6/6/22) – A study by the University of Michigan analyzed trends in interstate telehealth use by Medicare beneficiaries during 2017-2020, which covered the period both directly before and during the first year of the pandemic. The study found that the number of out-of-state telehealth services from the first quarter to the fourth quarter of 2020 increased by 572 percent, and that a higher percentage of out-of-state telehealth users lived in rural areas (28 percent). Additionally, 64 percent of out-of-state telehealth visits occurred between a patient and clinician in a bordering state. The study also found that most out-of-state telehealth use was for established patient care, suggesting the majority of out-of-state telehealth is used for continuity of care rather than acquisition of new patients.
Center for Connected Health Policy: State Telehealth Laws and Reimbursement Policies Report, Spring 2023 (5/16/23) – The Center for Connected Health Policy (CCHP) released its Spring 2023 Summary Report of state telehealth laws and Medicaid program policies. The Summary Report provides highlights on certain aspects of telehealth policy and the changes that have taken place between now and the previous edition, Fall 2022. The information for this summary report covers updates in state telehealth policy made between January and March 2023. Notably, the report found that 26 states have professional boards that issue special licenses or certificates or have exceptions to licensing requirements related to telehealth that may include registering with an in-state board rather than obtaining full licensure. Only Washington has added a cross state licensing exception since Fall 2022. However, this may be due to 2023 state legislation not yet being enacted at the time states were reviewed. Most of these states are not allowing for broad cross-state practice. The majority of the states that have added licensure exceptions in the past two years are for specific types of healthcare professionals in specific situations where the patient has moved or is visiting a certain state and has a pre-existing relationship with a provider in their former state. This has become a common issue of concern for college students wanting to continue care with their established mental health professionals in their home state, or for those that may be traveling for a limited amount of time.
Milbank Memorial Fund: Can Interstate Licensure Compacts Enhance the Health Care Workforce? (4/11/23) – Although health care licensing is traditionally a state function, rigid state borders can be ill-suited to meet needs in terms of access to care for underserved populations, emergency preparedness, and the changing nature of telemedicine-based care delivery. During the COVID-19 pandemic, at least 45 states waived or modified existing rules to allow health care practitioners to work across state lines through temporary licensure reciprocity. Policymakers and researchers are now debating options for longer-term licensure policy to mitigate the workforce crisis.
Politico Pro: States’ Experiment Helps Make Case for Easing Cross-State Licensure Rules (3/22/23) – A report from Cicero Institute found that telehealth did not spark more patient concerns than in-person care (read more in the research section). Many states waived licensing rules during the pandemic to allow their residents to meet with out-of-state doctors via telemedicine, and are now grappling with whether to continue to permit it. Telehealth lobbying groups like the Alliance for Connected Care have asked states to treat medical licenses like they do driver’s licenses, recognizing each other’s.
Stat News: How Cross-State Licensure Reform Can Ease America’s Mental Health Crisis (3/8/23) – Teletherapy has made mental health care more accessible than ever before, making care possible for people who otherwise would never have been able to get it. But the antiquated system of licensure in the United States is creating a huge barrier to realizing the potential for telehealth. Founder and CEO of Alma, Harry Ritter emphasizes the need for cross-state licensure reform now to address the needs of America’s growing mental health crisis and to ensure accessibility for everyone, regardless of their geographical location or identity.
The Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics at Harvard Law School – Achieving Telehealth’s Potential Webinar Series (March 2023)
- Achieving Telehealth’s Potential: The Federal Policy Landscape for Interstate Telehealth Practices. Prior to the pandemic, most states required a physician to be licensed in the state in which the patient is located, and reinstating this standard—which was among those relaxed during the COVID-19 crisis—will be a major deterrent to interstate telehealth use. This event, the first of three in a series, maped out the impact of our current physician licensure framework on the delivery of specialty care to patients through the patient, provider, and health system perspective.
- Achieving Telehealth’s Potential: The Federal Policy Landscape for Interstate Telehealth Practices. This event, the second of three in a series, mapped out the current and potential federal initiatives to facilitate interstate telehealth practices. Krista Drobac, Executive Director of Alliance for Connected Care, speaks in the panel.
- Achieving Telehealth’s Potential: The Federal Policy Landscape for Interstate Telehealth Practices. This event, the final of three in a series, explored some of the state leadership, challenges, and opportunities to build interstate telehealth practices.
Axios: States Eye Compacts, Scope of Practice Laws to Fill Holes in Health Workforce (2/2/23) – More states are working out differences over what medical services non-doctors can provide in order to ease stubborn workforce shortages plaguing health systems. The pandemic prompted states to waive certain licensure requirements which allowed providers to more easily practice in other states or to expand the services they were allowed to provide to patients, including via telehealth. However, without a permanent fix, health workers’ autonomy over patient care could conflict with the patchwork of state “scope of practice” laws.
Association of State and Territorial Health Officials (ASTHO): Telehealth and Licensure Policies Improving Healthcare Access for Rural Communities (1/26/23) – During the COVID-19 pandemic, states granted temporary waivers permitting telehealth licensure for out-of-state providers to deliver services in their own jurisdiction. ASTHO released a blog outlining the recent legislation at both the state and federal levels which has significantly affected the ability of health care providers to serve patients virtually and across state lines. The rapid adoption of telehealth during the COVID-19 pandemic, coupled with a renewed interest in cross-state licensure for providers, offer insights on how states can expand access to health care services, which is a central mission of public health departments.
Inside Telehealth: Interstate Compacts, Controlled Substance Prescribing, Payment Parity: Over 200 State Telehealth Bills Pre-Filed For 2023 (1/12/23) – More than 200 telehealth bills were pre-filed by states last year for the 2023 legislative session, including proposed laws letting states join interstate compacts, prescribing laws that include controlled substances, and payment parity laws. Interstate licensure is the next frontier for states in the expansion of telehealth. Cross-state licensing has been made available by interstate compacts, which an increasing number of states are attempting to join this year.
Inside Telehealth: FBI Misinterpreting Law, Slowing Interstate Telehealth (1/10/23) – Five interstate licensure compact leaders say the FBI is misinterpreting state laws that require federal background checks of providers, which is preventing, or slowing, states from joining interstate licensure compacts as demand for treatment across state lines via telehealth skyrockets with the recent two-year extension of most COVID-19 pandemic-era waivers. Confusion among compact leaders remains as they scramble to find a way to remedy the miscommunication on background checks and question whether proposed solutions would even be effective due to a lack of response from the FBI. Last Congress, Rep. Mann (R-KS) introduced the States Handling Access to Reciprocity for Employment Act to expedite and streamline the current licensing process and clarify any misconceptions surrounding background check requests. If reintroduced and passed, the legislation would in essence direct the FBI that if a state has a background check requirement because it has joined a state compact, the agency must approve the request eliminating some of local FBI’s discretion.
The Hill: State lines should no longer be barriers to health care (9/9/22) – Former VA Secretary David Shulkin penned an op-ed on how the VA expanded flexibility to provide care across state lines for Veterans, calling for this model to be replicated to benefit all Americans. The Veterans Administration has led the way in expanding the boundaries of care. While Sec. Shulkin was secretary, the VA changed outdated regulations that prevented veterans from accessing qualified providers simply because of geography. Veterans are now able to see their providers without regard to location.
Inside Telehealth: Cardiology, Family Physician Leaders: Continue Audio-Only Telehealth, Care Across State Lines (6/16/22) – During a recent FiscalNote webinar, leaders at the American College of Cardiology, and Alliance Advisory Board Member American Academy of Family Physicians (AAFP), expressed support for the federal government and states making pandemic-era allowances for telehealth across state lines and audio-only services permanent beyond the COVID-19 public health emergency. Members of the American College of Cardiology are invested in making sure patients with chronic heart conditions can see their regular provider via telehealth while traveling or spending part of their time in another state.
Inside TeleHealth: Medical Boards to Vote Saturday on New Telemedicine Policy (4/29/22) – The Federation of State Medical Boards is set to vote on its first update in nearly a decade to guidance on the appropriate use of telemedicine in the practice of medicine. The updated document contained sections related to licensure exceptions, standards of care, patient privacy, and health equity, among others. The Alliance for Connected Care submitted comments in response to the draft document in February, recommending that the FSMB consider broadening the circumstances in which it recommends interstate licensure for telehealth treatment.
Pharmacy Times: The Challenge of Multistate Pharmacy Licensure in the Telehealth Era (4/27/22) – Telehealth use expanded in pharmacies during the pandemic, however, pharmacy personnel face challenges when implementing these services, beginning with regulatory requirements affecting their ability to provide telehealth. Challenges for pharmacy personnel who wish to fully use telehealth to serve patients in multiple states include obtaining licenses to practice in each of these states. Acute shortages of pharmacists and pharmacy technicians in certain geographic regions and across areas of practice can be exacerbated by licensure requirements for such professionals. The American Society of Health-Systems Pharmacists (ASHP) has developed a series of policies that support the harmonization of laws and regulations impacting pharmacy practice across states and enhances the ability of pharmacists to practice in multiple states.
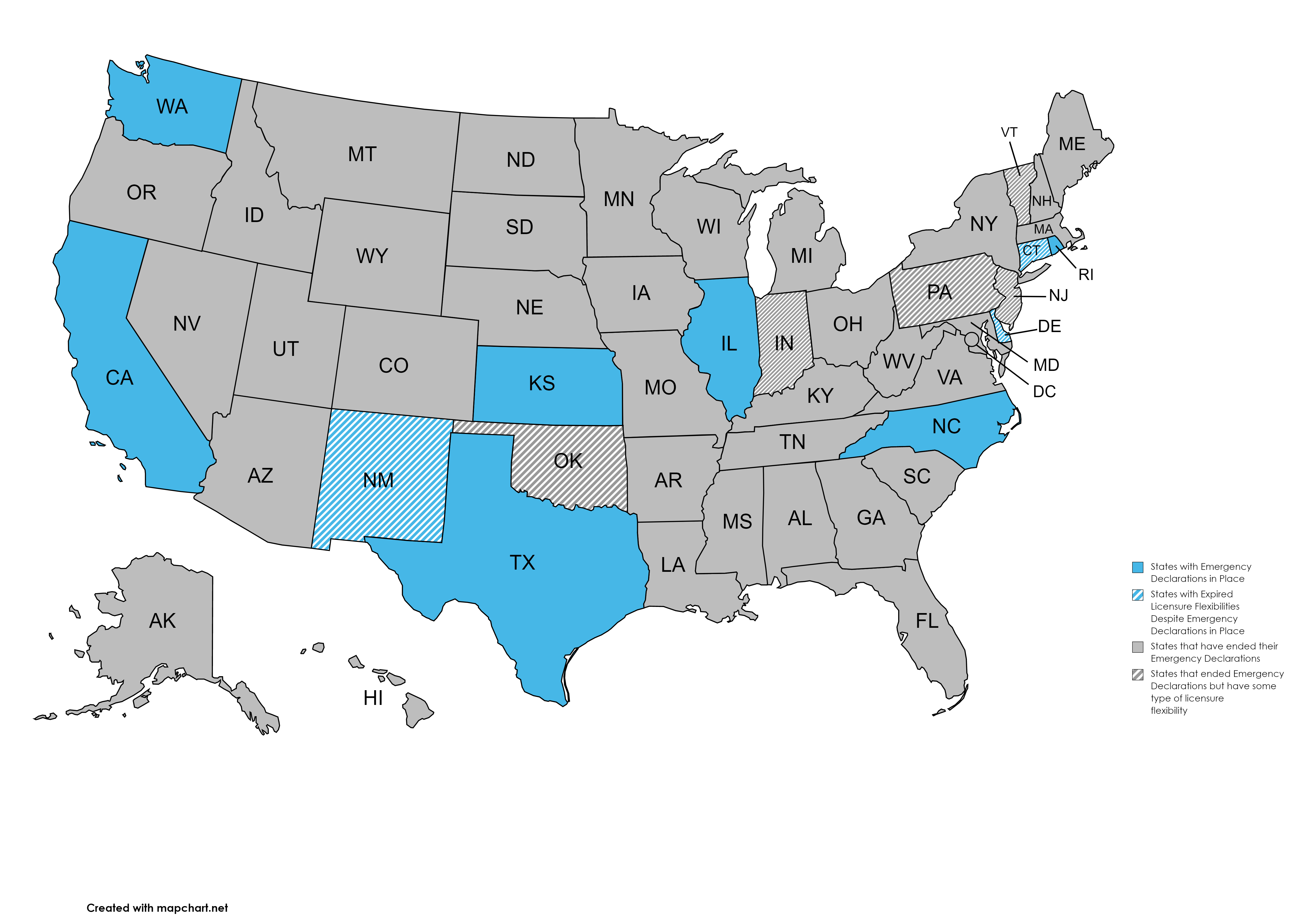
MedTech Intelligence: Telemedicine Moved Forward During the Pandemic. Our Policies and Regulations Need to Catch Up (4/22/22) – Outdated policies and regulations threaten to bring progress to a standstill, restrict vital telehealth access to millions of Americans, and exacerbate health inequities. All 50 states and the District of Columbia, as well as CMS, waived state licensure requirements so physicians could treat patients virtually across state lines during the pandemic. These flexibilities opened up a wave of record-breaking new investments in digital health technology, providing patients with new options in telehealth services and remote-monitoring solutions. However, according to a tracker by the Alliance for Connected Care, only 23 states still have those licensure waivers in place, and the future remains unclear for expanded telehealth benefit coverage and loosened prescription regulations. Permanently eliminating geographic and financial barriers to telemedicine is essential to reducing the health care access gap, providing consumers with greater choice in their medical care, and encouraging continued innovation in the digital health space.
Politico Pro: Telehealth growing pains (4/20/22) – The telehealth industry faces some uncertainty as more states end waivers allowing care across state lines. As many states’ emergency regulations permitting such care wind down and the patchwork system of state rules becomes patchier, millions of patients are losing expanded access to telehealth. The Alliance for Connected Care has proposed a voluntary national system, similar to the driver’s license system, that would enable states to recognize each other’s licenses. Patient advocates, public health officials and telehealth and provider groups are pushing for utilization of telehealth across state lines.
Politico Pro: Millions set to lose telehealth access across state lines as waivers wind down (4/19/22) – Millions of patients are losing expanded access to telehealth across state lines as many states’ pandemic emergency declarations wind down, prompting patient advocates, public health officials and telehealth and provider groups to call on states and Congress for a fix. According to data from the Alliance for Connected Care, states could see expanded access lapse in the second half of the year, with flexibilities intact for 15 states, down from 24 in early March. Access to virtual care across state lines, which patients increasingly took advantage of during the pandemic, is overwhelmingly popular among patients and providers. National data on the rise of care across state lines is sparse, but one in five providers say they provided care across state lines amid the pandemic, according to a recent Morning Consult poll conducted on behalf of the Alliance for Connected Care.
Additional articles worth a read!
- Forbes – Gas Prices Hurt People Going to the Doctor, But Interstate Telehealth Can Help (July 19, 2022)
- STAT – Sunsetting medical license reciprocity would return medicine to the dark ages (March 7, 2022)
- Progressive Policy Institute – Telehealth Saves Money and Lives: Lessons from the COVID-19 Pandemic (November 2021)
- BPC – What Eliminating Barriers to Interstate Telehealth Taught Us During the Pandemic (November 30, 2021)
- WSJ – Telehealth Rollbacks Leave Patients Stranded, Some Doctors Say (November 22, 2021)
- KHN/Time – Telehealth’s Limits: Battles Over State Lines and Licensing Threatens Patients’ Options (August 31, 2021)
- STAT – ‘The Party is winding down’: States and insurers resurrect barriers to telehealth, putting strain on patients (July 13, 2021)
- WSJ – A Cancer Patient’s Brutal Commute (July 12, 2021)
- Health Affairs – Mutual Recognition of Physician Licensure by States Would Provide for Better Patient Care (May 10, 2021)
- NEJM – Telemedicine and Medical Licensure – Potential Paths for Reform (February 25, 2021)
- JAMA Internal Medicine – The COVID-19 Pandemic – An Opportune Time to Update Medical Licensing (January 13, 2021)
- AJMC – Eliminating Barriers to Virtual Care: Implementing Portable Medical Licensure (October 17, 2019)
DC-MD-VA Reciprocity Agreement – On March 15, 2023, the District of Columbia Board of Medicine, Maryland State Board of Physicians, and Virginia Board of Medicine entered into an agreement to establish reciprocity amongst the parties to facilitate the expedited reciprocity licensure of physicians practicing within the three jurisdictions. A notice on the DMV Reciprocity Pathway from the DC Health, Health Regulation and Licensing Administration noted the following: “We understand that obtaining a license can be a lengthy process for physician applicants and due to the close proximity and geographical relationship of the District of Columbia, Maryland, and Virginia, many physicians need licensure in all three (3) jurisdictions. The purpose of the expedited pathway allows the Board to minimize the administrative burden on the applicant and staff, while still concurrently ensuring minimum qualifications are met to protect the public.”
Additional information on this new pathway from the respective Boards can be found below:
- DC
- Maryland
- Virginia
In 2022, the Uniform Law Commission made available to states model legislation called the Uniform Telehealth Act, which aims to give states the clear guidance and framework they need to facilitate the delivery of services via telehealth consistent with the standard of care of the state in which the patient is located. In recent years, improvements in telecommunication technologies have transformed the delivery of health care. The arrival of the COVID-19 pandemic greatly expanded patient demand for telehealth services. To meet patient needs, many states chose to modify licensure and other requirements that served as barriers to the delivery of telehealth services. Today, many states are re-examining laws related to telehealth, often with an eye toward expanding access to care while maintaining protections for patients.
The Uniform Telehealth Act has two broad goals. The first is to make clear that, as a general matter, health care services may be provided through telehealth, if doing so is consistent with applicable professional practice standards and the practitioner’s scope of practice, as defined by the state in which the patient is located. The Telehealth Act’s second goal is to establish a registration system for practitioners who hold licenses in other states. This act permits a registered practitioner to provide telehealth services to patients located in the state adopting the act. The ULC hopes the Act will give states the clear guidance and framework they need to implement effective telehealth services, as well as open borders so that more practitioners are able to assist patients that might otherwise have limited access to health care.
Harvard Law School: Alliance Executive Director Speaks on Interstate Telehealth Panel (3/9) – Krista Drobac, Executive Director of Alliance for Connected Care, joined an esteemed panel at the Harvard Law School’s Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics’ event on the federal policy landscape for interstate telehealth practices. Prior to the pandemic, most states required a physician to be licensed in the state in which the patient is located, and reinstating this standard—which was among those relaxed during the COVID-19 crisis—will be a major deterrent to interstate telehealth use. Patients will have to drive across state lines to have virtual consults with specialized experts, and providers will be dissuaded from developing truly national telehealth practices. More information on the Alliance’s work on this issue can be found here.
Alliance for Connected Care: Alliance Statement on Cross-State Licensure as SOTU Priority Issue (2/7) – On February 7, the Alliance for Connected Care released a statement in advance of President Biden’s State of the Union address:
“We are grateful to President Biden for highlighting the pressing issue of cross-state licensure in advance of the State of the Union. The pandemic taught us that it is possible, and safe, to allow providers to treat patients anywhere. State borders should cease to be an artificial barrier to health care. It’s time to change the cumbersome, time-consuming, expensive, and duplicative licensing rules that prevent patients from receiving care from qualified, licensed providers in other states. We would miss an opportunity if we approach this issue incrementally. Allowing cross-state treatment for one patient population or disease-type may have made sense as a first step before the pandemic, but we have had more than two years of access for patients in need of all types of services. We should change the status quo for all patients, regardless of diagnosis.”
Featured Advocacy: Letter to Governors on Care Across State Lines
On November 1, 2021, more than 230 organizations sent a letter to all 50 state governors urging them to maintain and expand licensure flexibilities enacted at the start of the pandemic for the duration of the federal public health emergency, to better address patient needs during the ongoing pandemic. The letter was convened by the Alliance for Connected Care, ALS Association, and National Organization for Rare Disorders (NORD), and includes a diverse mix of signers ranging from patient advocacy organizations, hospitals and health systems, academic medical centers, higher education, digital health companies, health information management associations, and many more.
 Loading...
Loading...