Share This Study!
Fall 2022
The Alliance for Connected Care commissioned an independent Medicare claims data analysis to better understand telehealth utilization and the potential financial impact of long-term telehealth expansion on the Medicare program. As expected, the findings of this analysis align with the individual experiences and data collected by Alliance for Connected Care members.
“It’s hard to break conventional wisdom in Washington. We finally have comprehensive telehealth utilization data in Medicare that should rectify the misconception that telehealth is somehow uniquely subject to over-use.” – Krista Drobac, Alliance for Connected Care
The research project, executed by Teus Health, fully analyzed Medicare fee-for-service claims data[1] across three full years – 2019, 2020, and 2021 – to answer and further explore the following crucial questions:
- Is telehealth adding to the total volume of Medicare services or replacing in-person services?
- Compared to patients who had an initial in-person visit, did patients who had a telehealth visit have more follow-up visits?
We expect this research to be useful to the Congressional Budget Office, MedPAC, and other entities which have expressed concerns that telehealth legislation may lead to additional costs for the Medicare program.
Finding 1: There is no evidence that telehealth is adding to the total volume of Medicare services.
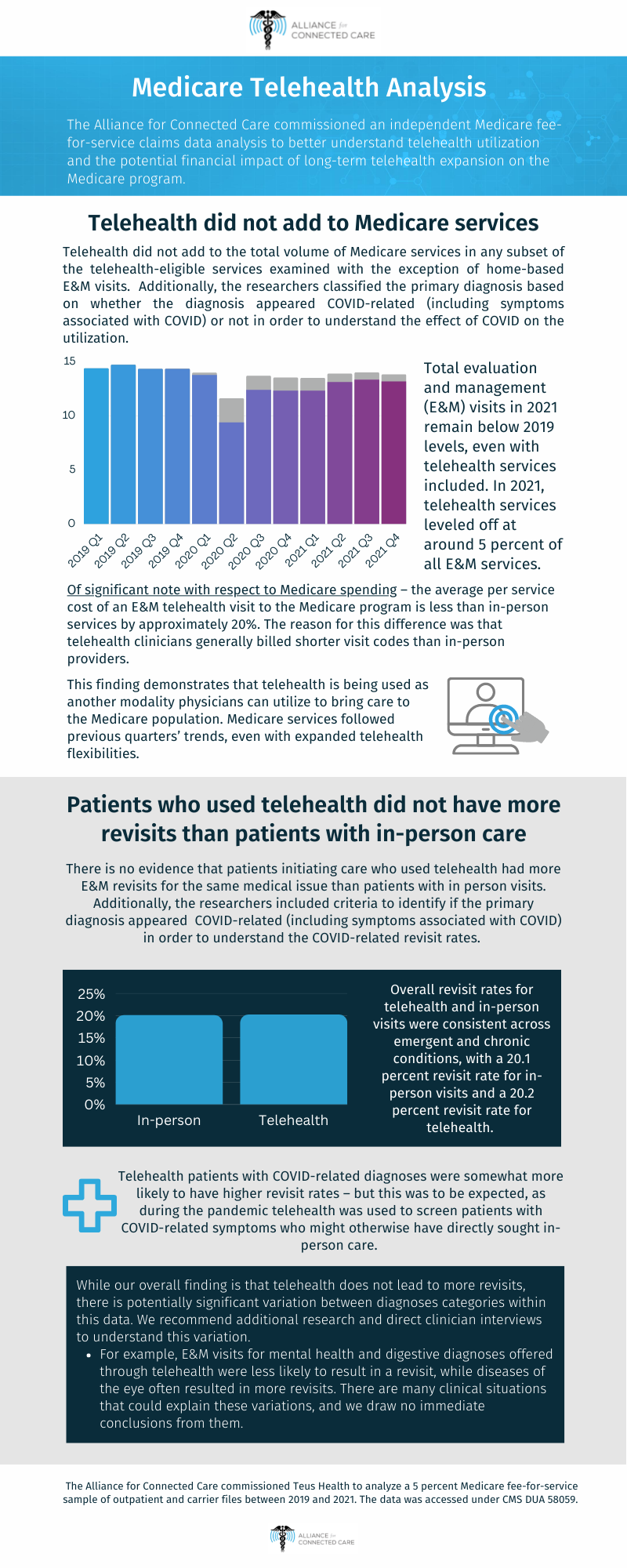
The analysis examined the utilization of services to determine better understand if telehealth is adding to the total volume of Medicare services or replacing in-person services. Additionally, the researchers classified the primary diagnosis based on whether the diagnosis appeared Covid-related (including symptoms associated with Covid) or not in order to understand the effect of COVID on the utilization.
- Total evaluation and management (E&M) visits in 2021 remain below 2019 levels, even with telehealth services included. In 2021, telehealth services leveled off at around 5 percent of all E&M services.
[1] Source: Medicare 5% sample, outpatient and carrier files, 2019-2021, accessed under CMS DUA 58059.
- Telehealth did not add to the total volume of Medicare services in any subset of the telehealth-eligible services examined with the exception of home-based E&M visits. Telehealth continues to represent a larger percentage of home visits than overall E&M visits.
- Of significant note with respect to Medicare spending – the average per service cost of an E&M telehealth visit to the Medicare program is less than in-person services by approximately 20%. The reason for this difference was that telehealth clinicians generally billed shorter visit codes than in-person providers.
- Provider types most heavily relying on telehealth included all mental health and substance use disorder providers, primary care clinicians, as well as endocrinologists, pain management, anesthesiology, and sleep medicine specialties.
- This finding demonstrates that telehealth is being used as another modality physicians can utilize to bring care to the Medicare population. Medicare services followed previous quarters’ trends, even with expanded telehealth flexibilities.
Finding 2: There is no evidence that patients initiating care who used telehealth had more E&M revisits for the same medical issue than patients with in-person visits.
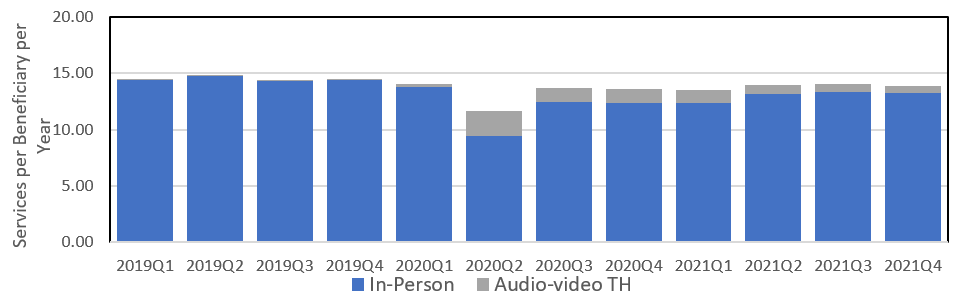
The analysis examined revisit rates to answer whether patients who had a telehealth E&M visit had more follow-up visits than patients who had an initial in-person visit. Additionally, the researchers included criteria to identify if the primary diagnosis appeared COVID-related (including symptoms associated with COVID) in order to understand the COVID-related revisit rates.
-
- Overall revisit rates for telehealth and in-person visits were consistent across emergent and chronic conditions, with a 20.1 percent revisit rate for in-person visits and a 20.2 percent revisit rate for telehealth.
- Telehealth patients with COVID-related diagnoses were somewhat more likely to have higher revisit rates – but this was to be expected, as during the pandemic telehealth was used to screen patients with COVID-related symptoms who might otherwise have directly sought in-person care.
- While our overall finding is that telehealth does not lead to more revisits, there is potentially significant variation between diagnoses categories within this data. We recommend additional research and direct clinician interviews to understand this variation.
- For example, E&M visits for mental health and digestive diagnoses offered through telehealth were less likely to result in a revisit, while diseases of the eye often resulted in more revisits. There are many clinical situations that could explain these variations, and we draw no immediate conclusions from them.
See the analysis below or here.
 Loading...
Loading...