Alliance Telehealth Data Strategy (Updated for 2022)
Building on our important work as part of the Taskforce on Telehealth, and ongoing discussions with policymakers around the implications of permanent telehealth expansion, the Alliance for Connected Care continues to collect data on utilization, costs, etc. We seek to understand what we have learned about telehealth utilization and its effect on prevention, urgent care, transportation, and more. Our goal is to educate a conversation about what impact expanding telehealth access in Medicare will have on federal budgeting models.
This work has three primary components –
- Independent research on telehealth utilization in Medicare Fee-for-Service to demonstrate its relationship (or lack of one) to total cost of care. We are currently in the funding phase of this work, but hope to publish in mid-2022. Contact cadamec@connectwithcare.org if you are interested in supporting this work and would like the details of the proposal.
- Collection of organization-specific data and charts on telehealth. In our efforts to gather data on cost, we are asking organizations, health systems, and/or providers to submit data on telehealth during COVID-19. The Alliance has regularly shared information from our members, partners, and contributors with leading policymakers on core issues of importance – such as:
- Utilization Data: to what extent is telehealth serving as a replacement for in-person care?
- No-show Rates: Were no-show rates reduced, and if so, by how much?
- Post-discharge: Were post-discharge transition codes (99495 and 99496) billed at a higher rate?
- SNF Transfers: Did telehealth resolve skilled nursing facility-resident issues without transfer, i.e. were transfers to hospitals lower without compromising patient care?
- Demographics/Race/Ethnicity/Age Distribution: To show telehealth utilization broken down by various demographics including race/ethnicity, age, gender, income, education, etc.
(This content is shared among Alliance members and policymakers, but not published without explicit permission)
- Collection and dissemination of third-party telehealth research. The Alliance for Connected Care’s Studies and Surveys page includes an extensive list of major telehealth studies — and we are adding more every week. Please feel free to flag your work for inclusion on this page and in our weekly newsletter (which captures and shares new research as it is published).
Please submit your data/research to rikki.cheung@connectwithcare.org. We will be sure to attribute any data. Examples of the types of data/graphs/charts we are looking for are below. Please feel free to reach out with any questions or more examples.
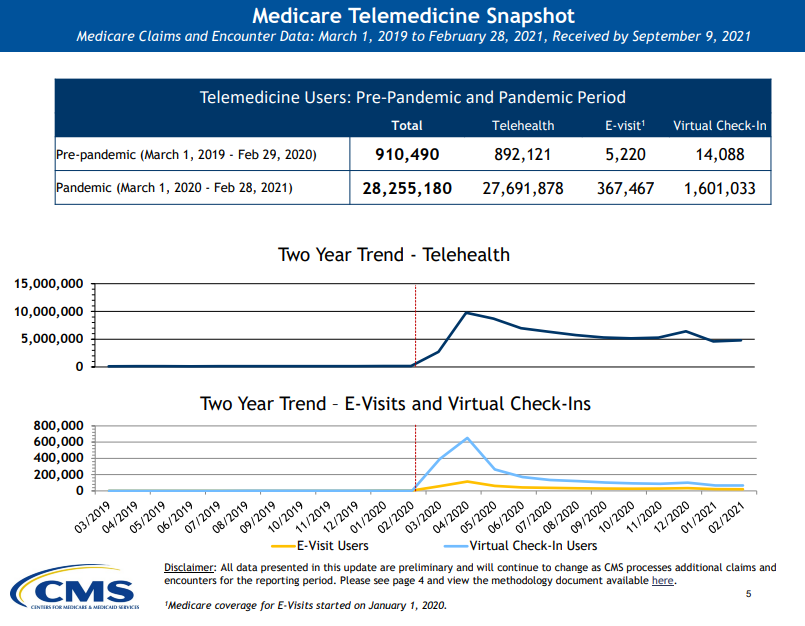
Source: CMS Medicare Telemedicine Data Snapshot
Suggested Research Cohort Structure
Planning to submit data to the Alliance? Here are some model research recommendations to follow, if possible, for the best alignment with our members:
#1 – Primary Care Only
Longitudinal cohort analysis of Medicare FFS beneficiaries who had a PCP visit in CY2019 and at least one PCP visit in CY2020 and CY2021.
- Overall framework:
- Medicare FFS primary care established E&M visits in 2019 and their activity following their first PCP visit in CY2019 through 12/31/2021 to establish per patient visit rates per calendar year and per 6 month period (Jan-Jun, Jul-Dec). Demographic summaries will be provided, including sex, race, ethnicity, and age group (65-69, 70-74, 75-79, 80-84, 85+). Per person visits rates will be calculated for total visits, in-person visits, and virtual visits. Analysis will be repeated by categorizing patients into visit frequency categories of 1 visit per calendar year, 2-3 visits per calendar year, and 4+ visits per calendar year, and then recalculating per person visit rates.
- Data definitions and criteria:
- Primary care filter based on MGMA specialty designation of primary care provider
- Established E&M visit criteria based on including one of the below codes as well as a virtual ‘flag’ for their encounter:
- Est. E&M visit codes: 59430, 92002, 92004, 92012, 92014, 98966, 98967, 98968, 98969, 98970, 98971, 98972, 99024, 99211, 99212, 99213, 99214, 99215, 99241, 99242, 99243, 99244, 99245, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99318, 99354, 99391, 99392, 99393, 99394, 99395, 99396, 99397, 99421, 99422, 99423, 99441, 99442, 99443, 99444, 99455, 99456, 99468, 99469, 99471, 99472, 99475, 99476, 99477, 99478, G0101, G0246, G0337, G0425, G0426, G0427, G0438, G0439, G0445, G0449, G0468, G0509, G2082, G2083, G2214, G2250, G9156, G9685, S0257, S0260, S0612, S0613, S0622, S5190, S9200, T1015, T1024, T1025, T1026, 0510, 0511, 0514, 0515, 0517, 0519, 0520, 0521, 0523, 0529, 0530, 0531, 0560, 0561, 0770
- Virtual flag criteria:
- to be designated as a virtual telephone visit: a code of 99441, 99442, 99443, G0071, G2012 and the absence of modifiers of GT and 95
- to be designated as a virtual video visit: the modifiers of GT, 95, GQ, or G0, or a place of service code of 02
- Ideally, future analyses will include risk adjustment, acute and ED utilization per 1000 visits, and more granular visit reasons.
This framework excluded beneficiaries under the age of 65 from this analysis in addition to exclusions of beneficiaries with a COVID diagnosis or mortality in calendar years 2019-2021.
#2 – Primary and Specialty Care
Longitudinal cohort analysis that is similar to the above, but doesn’t limit to primary care. Criteria for data pull includes:
- Medicare FFS only
- Patients with visits (any type of ambulatory visit in any medical discipline) in each of the years (2019, 2020, 2021); main goal here is that this supports the “they are sticky to your institution” argument (i.e., not institutionally shopping)
- Not deceased
- Breakdown of per unique patient in person + virtual care use (visits per member per year and per 6 month periods)
- Visits per unique patient by some groupers to create 6 filters on the stacked column
- In person and virtual
- Primary Care
- Mental Health
- Specialty
- In person and virtual
- Visits per unique patient by some groupers to create 6 filters on the stacked column
- This would bring specificity to existing health system data, but narrow to FFS only, filtered further to a “patients with visits each year” metric, eliminate deceased patients, and then go from just in person vs telemedicine to in person vs telemedicine breakdowns for primary, mental health, and specialty care.
Other Data Questions
The following are other areas of interest where we welcome data on, with some overlap with the top questions listed above:
- SNF transfers and use of transition codes
- Percentage of times you could address uses without SNF transfers
- Reasons for transfers
- Higher rate of transition codes with telehealth use?
- Understanding sicker patient mix/acuity and its impacts on the data
- Longitudinal look at patient mix
- Does the panel reflect the same group of patients over time? Are patients coming and going from the panel over time? (i.e., leakage and keepage)
- Virtual user cohort vs. non-virtual user cohort
- Time limit from 2019 – 2021, with individuals who had one visit of any kind in each of these three years to evaluate change over time
- Codes of specific concerns and types of visits telehealth is substituting for, along with any indication for the reason for the visit
- Virtual care and follow-up rates
- Did a telehealth visit lead to an in-person visits for the same condition?
- Was a telehealth visit used as a follow-up to an in-person visit?
- Incorporating risk scores/risk adjustment into a longitudinal panel