State Expansion of Telehealth and Licensing Waivers
During the public health emergency, all 50 states and the District of Columbia used emergency authority to waive some aspect(s) of state licensure requirements to facilitate patients getting care. This has provided an unprecedented opportunity for patients, providers, and policymakers to explore the impact of cross-state care. This has benefited the delivery of health care in many ways, but perhaps most notably, it has opened up many new avenues for patient choice and access to care.
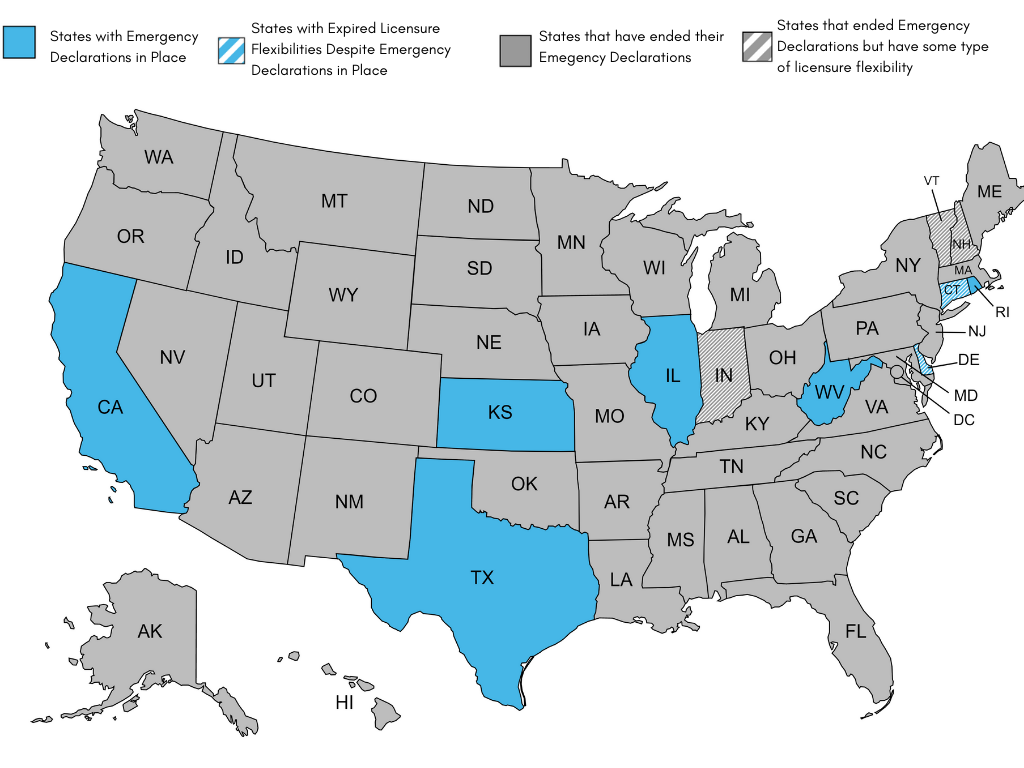
As states begin to lift their COVID-19 emergency waivers or let them expire, many of the telehealth and licensure flexibilities enacted at the start of the pandemic to ensure continuity and access to care for patients are also expiring. As such, the Alliance has created a chart outlining which states have lifted their COVID-19 emergency waivers, and how this has impacted telehealth and licensing flexibilities in each state. This document is no longer updating this document after its last updated date given most states have or plan to terminate their emergency declarations. It was last updated on December 16, 2022.
As of December 16, 2022:
- 42 states and D.C. have ended their emergency declarations: AL, AK, AZ, AR, CO, DC, FL, GA, HI, ID, IN, IA, KY, LA, ME, MD, MA, MI, MN, MS, MO, MT, NE, NV, NH, NJ, NM, NY, NC, ND, OH, OK, OR, PA, SC, SD, TN, UT, VT, VA, WA, WI, WY.
- IN, NH, and VT, however, have licensure flexibilities still in place.
- IN will extend out-of-state health care registry through the duration of the federal PHE.
- NH SB 277 extends the expiration for temporary and emergency licenses for health care workers, if they were obtained on or before Jan. 31, 2022, through June 30, 2023.
- VT passed legislation that extends pandemic-era license waivers through June 30, 2023.
- IN, NH, and VT, however, have licensure flexibilities still in place.
- 8 states continue to have emergency declarations in place: CA, CT, DE, IL, KS, RI, TX, WV.
- Of these 8 states, 6 states still have licensure flexibilities in place. Licensure flexibilities have expired in CT and DE, despite emergency declarations still in place.
- CA is going through a phased rollback of COVID-era waivers, however waivers on telehealth and licensure are still in place.
- In total, 9 states still have licensure flexibilities in place.
Note: The Alliance is no longer updating this document after its last updated date given most states have or plan to terminate their emergency declarations. It was last updated on December 16, 2022.
Figure 1. Map highlighting status of COVID-era telehealth and licensure waivers state-by-state. Last updated December 16, 2022.
 Loading...
Loading...
 Loading...
Loading...
CMS Approved 1135 Waivers
Under a disaster or emergency declaration and a public health emergency, the HHS Secretary is authorized to take additional actions to provide programmatic flexibility in Medicare, Medicaid and the Children’s Health Insurance Program through section 1135 waivers. The Secretary may issue blanket waivers, or may approve state specific waivers. Waivers end no later than the termination of the emergency period. CMS released a checklist for states to aid in the development of 1135 waivers requests.
COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers
Several states requested flexibility to incent greater use of telehealth through Medicaid Section 1135 Waivers during the pandemic. For example:
- IL, LA, NC, and WA requested CMS to allow providers to use non-HIPAA compliant telehealth modes from platforms like Facetime, WhatsApp, and Skype to facilitate visits.
- CA requested flexibility to make it easier for providers to care for people in their own homes by allowing telehealth and virtual/telephonic communications for covered State plan benefits, a Waiver of face-to-face encounters for FQHCs and Rural Health Clinics, and Reimbursement of virtual communication and e-consults for certain providers.
- MD requested flexibility so that Medicaid and Managed care enrollees could use telephones to receive care if they did not have an appropriate device.
- SD requested flexibility to allow Medicaid to pay for the same telehealth services that Medicare has been granted authority to pay for, including services furnished while a patient is at home.
As of April 2020, CMS had approved 53 state waivers. A full list of the approved 1135 waivers (last updated April 23, 2020) can be found here.