Summary: Proposed CY 2023 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS 1772-P)
Summary: Proposed CY 2023 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS 1772-P)
On July 15, 2022, the Centers for Medicare & Medicaid Services (CMS) released the CY2023 Medicare Hospital Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Center (ASC) Payment System Proposed Rule, which makes policy and payment updates for hospital outpatient and ambulatory surgical centers. The proposed rule aims to advance health equity and improve access to care in rural communities by establishing policies for Rural Emergency Hospitals (REH), and provides for payment for certain behavioral health services furnished via communications technology.
CMS is seeking comment on several measures under consideration for the new Rural Emergency Hospital Quality Reporting (REHQR) Program, as well as on topics of interest for the REHQR Program for future rulemaking, including rural behavioral/mental health, rural maternal health, and rural telehealth services.
This proposed rule will have a 60-day comment period, which will end on September 13, 2022. The final rule will be issued in early November. See here for a press release, general fact sheet, fact sheet on the Rural Emergency Hospitals Proposed Rulemaking, and the proposed rule.
Below is a summary of key telehealth provisions included within the proposed rule. Specific information that CMS is requesting comments on are also included below.
Nonrecurring Policy Changes – Mental Health Services Furnished Remotely by Hospital Staff to Beneficiaries in Their Homes
- CY 2023 OPPS Proposal to Pay for Mental Health Services Furnished Remotely by Hospital Staff
a. Designation of Mental Health Services Furnished to Beneficiaries in Their Homes as Covered OPD Services
During the PHE for COVID-19, many beneficiaries may be receiving mental health services in their homes from a clinical staff member of a hospital or Critical Access Hospital (CAH) using communications technology under the flexibilities that CMS adopted to permit hospitals to furnish these services. After the PHE ends, absent changes to CMS regulations, the beneficiary would need to physically travel to the hospital to continue receiving these outpatient hospital services from hospital clinical staff. Given the changes in payment policy for mental health services via telehealth by physicians and practitioners under the Physician Fee Schedule (PFS) and mental health visits furnished by staff of RHCs and FQHCs, using interactive, real-time telecommunications technology, it is important to maintain consistent payment policies across settings of care so as not to create payment incentives to furnish these services in a specific setting.
- CMS proposes to designate certain services provided for the purposes of diagnosis, evaluation, or treatment of a mental health disorder performed remotely by clinical staff of a hospital using communications technology to beneficiaries in their homes as hospital outpatient services that are among the “covered hospital outpatient department (OPD) services” designated by the Secretary as described in section 1833(t)(1)(B)(i) of the Act and for which payment is made under the OPPS. To effectuate payment for these services, CMS proposes to create OPPS-specific coding to describe these services. The proposed code descriptors specify that the beneficiary must be in their home and that there is no associated professional service billed under the PFS. CMS notes that, consistent with the conditions of participation for hospitals at 42 CFR 482.11(c), all hospital staff performing these services must be licensed to furnish these services consistent with all applicable State laws regarding scope of practice.
- CMS also proposes that the hospital clinical staff be physically located in the hospital when furnishing services remotely using communications technology for purposes of satisfying the requirements at 42 CFR 410.27(a)(1)(iii) and § 410.27(a)(1)(iv)(A), which refer to covered therapeutic outpatient hospital services incident to a physician’s or nonphysician practitioner’s service as being “in” a hospital outpatient department.
- CMS is seeking comment on whether requiring the hospital clinical staff to be located in the hospital when furnishing the mental health service remotely to the beneficiary in their home would be overly burdensome or disruptive to existing models of care delivery developed during the PHE, and whether they should revise the regulatory text in the provisions cited above to remove references to the practitioner being “in” the hospital outpatient department.
- CMS also proposes to assign HCPCS codes CXX78 and CXX79 to APCs based on the PFS facility payment rates for CPT codes 96159 (Health behavior intervention, individual, face-to-face; each additional 15 minutes (List separately in addition to code for primary service)) and 96158 (Health behavior intervention, individual, face-to-face; initial 30 minutes), respectively.
- CMS is seeking comment on the designation of mental health services furnished remotely to beneficiaries in their homes as covered OPD services payable under the OPPS, and on these proposed codes, their proposed descriptors, the proposed HCPCS codes and PFS facility rates as proxies for hospital costs, and the proposed APC assignments for the proposed codes. CMS notes this proposal would also allow these services to be billed by CAHs, even though CAHs are not paid under the OPPS.
b. Periodic In-Person Visits
In the CY 2022 PFS final rule, CMS finalized that, after the first mental health telehealth service in the patient’s home, there must be an in-person, non-telehealth service within 12 months of each mental health telehealth service—but also finalized a policy to allow for limited exceptions to the requirement. Specifically, if the patient and practitioner agree that the benefits of an in-person, non-telehealth service within 12 months of the mental health telehealth service are outweighed by risks and burdens associated with an in-person service, and the basis for that decision is documented in the patient’s medical record, the in-person visit requirement will not apply for that 12-month period (86 FR 65059). CMS finalized identical in-person visit requirements for mental health visits furnished through communications technology for RHCs and FQHCs.
- In the interest of maintaining similar requirements between mental health visits furnished by RHCs and FQHCs via communications technology, mental health telehealth services under the PFS, and mental health services furnished remotely under the OPPS, CMS proposes to require that payment for mental health services furnished remotely to beneficiaries in their homes using telecommunications technology may only be made if the beneficiary receives an in-person service within 6 months prior to the first time the hospital clinical staff provides the mental health services remotely; and that there must be an in-person service without the use of telecommunications technology within 12 months of each mental health service furnished remotely by the hospital clinical staff.
- CMS also proposes the same exceptions policy as was finalized in the CY 2022 PFS final rule, specifically, that would permit exceptions to the requirement that there be an in-person service without the use of communications technology within 12 months of each remotely furnished mental health service when the hospital clinical staff member and beneficiary agree that the risks and burdens of an in-person service outweigh the benefits of it. Exceptions to the in-person visit requirement should involve a clear justification documented in the beneficiary’s medical record including the clinician’s professional judgement that the patient is clinically stable and/or that an in-person visit has the risk of worsening the person’s condition, creating undue hardship on the person or their family, or would otherwise result in disengaging with care that has been effective in managing the person’s illness.
- In the interest of continuity across payment systems so as to not create incentives to furnish mental health services in a given setting due to a differential application of additional requirements, and to avoid any burden associated with immediate implementation of the proposed in-person visit requirements, CMS proposes that the in-person visit requirements would not apply until the 152nd day after the PHE for COVID-19 ends.
c. Audio-only Communication Technology
During the PHE, CMS used waiver authority under section 1135(b)(8) of the Act to temporarily waive the requirement, for certain behavioral health and/or counseling services for audio-only E/M visits, that telehealth services must be furnished using an interactive telecommunications system that includes video communications technology, allowing for payment for services furnished using audio-only communications technology. In order to maximize accessibility for mental health services, particularly for beneficiaries in areas with limited access to broadband infrastructure, and in the interest of policy continuity across payment systems so as to not create incentives to furnish mental health services in a given setting due to a differential application of additional requirements, CMS proposes a similar policy for mental health services furnished remotely by hospital clinical staff to beneficiaries in their homes through communications technology.
- Specifically, CMS proposes that hospital clinical staff must have the capability to furnish two-way, audio/video services but may use audio-only communications technology given an individual patient’s technological limitations, abilities, or preferences.
Other Relevant Telehealth Provisions:
Request for Comment on Additional Measurement Topics and for Suggested Measures for REH Quality Reporting
CMS’ request for information in the CY 2022 OPPS/ASC proposed rule yielded suggested additional topics for quality measures appropriate to the REH setting. CMS requests comment on the below additional topics and requests suggestions for specific measures to assess the patient experience, outcome, and processes related to these topics. In addition, CMS requests comment on other potential topics not listed that would be applicable to an REH quality reporting program.
- Telehealth. CMS is seeking public comment on potential future quality measures development to address quality of care using telehealth services in rural and rural emergency settings; as well as, on the ways in which REHs could utilize telehealth and telemedicine to bridge both gaps in expertise and distance to render quality care services.
- Mental Health. CMS is seeking public comment on potential future quality measures for behavioral health services in rural and rural emergency settings, and on the ways in which REHs could utilize telehealth and telemedicine to bridge both gaps in expertise and distance to render quality behavioral health care services.
- ED Services. CMS is seeking public comment on potential future quality measures for emergency care services in rural and rural emergency settings, and on the ways in which REHs could utilize telehealth and telemedicine to bridge both gaps in expertise and distance to render quality of care.
- Equity. CMS is seeking public comment on potential future quality measures for health equity in rural and rural emergency settings, and on the ways in which REHs could utilize telehealth and telemedicine to bridge both gaps in expertise and distance to render equitable, quality of care.
Summary: Proposed Calendar Year 2023 Physician Fee Schedule
Summary: Proposed Calendar Year 2023 Physician Fee Schedule
On July 7, 2022, CMS issued the Calendar Year 2023 (CY2023) Physician Fee Schedule (PFS) proposed rule, which makes payment and policy changes under Medicare Part B.
CMS is proposing to add some services to the Medicare Telehealth Services List on a Category 3 basis through the end of 2023, some of which had not been previously added to the Medicare Telehealth List during the COVID-19 public health emergency (PHE), but will be added on a subregulatory basis.
In addition, CMS is proposing that Medicare telehealth services furnished on or before the 151st day after the end of the PHE, in alignment with the extensions of telehealth-related flexibilities in the Consolidated Appropriations Act (CAA), 2022, will continue to be processed for payment as Medicare telehealth claims when accompanied with the modifier “95”. CMS is also proposing that physicians and practitioners can continue to report the place of service code that would have been reported had the service been furnished in-person during the 151-day period after the end of the PHE, as finalized on an interim basis in the March 31 IFC (85 FR 19233).
Below is a summary of key payment and policy change proposals within the proposed rule. Specific information that CMS is requesting comments on are also included below. Comments are due September 6, 2022.
See here for a press release, general fact sheet, fact sheet on the Medicare Shared Services Program, fact sheet on the Quality Payment Program, and blog on behavioral health changes that accompanied the proposed rule.
- Provisions of the Proposed Rule for the PFS
- Payment for Medicare Telehealth Services Under Section 1834(m) of the Act
- Payment for Medicare Telehealth Services Under Section 1834(m) of the Act
- Requests to Add Services to the Medicare Telehealth Services List for CY 2023
- CMS found that none of the requests received by the February 10th submission deadline met Category 1 or Category 2 criteria for permanent addition to the Medicare telehealth services list. As a reminder, Category 1 are services that are similar to professional consultations, office visits, and office psychiatry services that are currently on the Medicare Telehealth Services list, and the criterion for adding services under Category 2 is that there is evidence of clinical benefit if provided as telehealth.
- CMS also assessed the appropriateness of adding the proposed services to the Medicare Telehealth Services List on a Category 3 basis instead. CMS is not proposing changes to the length of time the services included on the temporary Category 3 basis. Category 3 will continue to be included through the end of CY 2023. In the event the PHE extends into CY 2023, CMS may consider revising this policy.
- CMS is proposing to add some services to the Medicare Telehealth Services List on a Category 3 basis through the end of 2023, some of which CMS had not previously added to the Medicare Telehealth List during the PHE, but will be added on a subregulatory basis as provided in § 410.78(f) of its regulations. CMS has received information from interested parties suggesting potential clinical benefit for some of these services. For other services, CMS believes there is sufficient evidence of potential clinical benefit to warrant allowing additional time for interested parties to gather data to support their possible inclusion.
- CMS is proposing to continue to allow certain telehealth services that would otherwise not be available via telehealth after the expiration of the PHE to remain on the Medicare Telehealth Services List for 151 days after the expiration of the PHE, as per the Consolidated Appropriations Act, 2022 (CAA, 2022) (Pub. L. 117-103, March 15, 2022).
- CMS is proposing that CPT codes 97150, 97530, and 97542 (the set of therapy services that are currently on the Medicare Telehealth Services List on a temporary basis for the PHE), should be added to the Medicare Telehealth Services List through the end of CY 2023 on a temporary, Category 3 basis. This will allow CMS time to gather additional data that could support the inclusion on a more permanent basis. CMS also believes keeping these services through the end of CY 2023 would preserve access to care and promote health equity, and based on information provided by interested parties, internal review, may safely be furnished as telehealth outside of the circumstances of the PHE through the end of CY 2023.
- CMS is encouraging commenters to supply additional information in support of adding other requested therapy services, namely CPT codes 97537, 97763, 90901, and 98960-98962, to the Medicare Telehealth Services List on a permanent basis, including information regarding the safety and appropriateness of furnishing these services via telehealth. Including these services on the Medicare Telehealth Services List during the PHE and through CY 2023 would allow additional time for the development of evidence for CMS to consider when evaluating these services for potential permanent addition to the Medicare Telehealth Services List on a Category 1 or 2 basis.
- As noted in the CY 2021 PFS final rule (85 FR 84535), CMS will assign the Telephone E/M visit codes (CPT codes 99441, 99442, and 99443) a “bundled” status after the end of the PHE and the 151-day extension period. CMS will post the RUC-recommended RVUs for these codes in accordance with the usual practice.
- CMS is seeking comment on whether GI Tract Imaging, CPT code 91110 and Ambulatory Continuous Glucose Monitoring, CPT code 95251 would meet the criteria for inclusion on the Medicare Telehealth Services List either for the PHE, as Category 3 services, or permanently on a Category 1 or 2 basis as whether they are inherently non-face-to-face services, and therefore, may not fit within the scope of services that could be furnished as Medicare telehealth services. CMS is also seeking comment on whether these services would involve an in-person service when furnished without the use of telecommunications system.
- CMS is proposing to add CPT codes 95970, 95983, and 95984 to the Medicare Telehealth Services List on a Category 3 basis. CMS is concerned about CPT codes 95970, 95983, and 95984, which describes general brain nerve neurostimulation, about whether the full scope of service elements could be furnished via two-way, audio-video communication technology, particularly since it is unclear whether the connection between the implanted device and the analysis/calibration equipment can be done remotely. CMS is also soliciting comment on their concerns regarding patient safety and whether these services are appropriate for inclusion on the Medicare Telehealth Services List outside the circumstances of the PHE.
- CMS is soliciting comments on patient safety concerns regarding emotional/behavior assessment, psychological, or neuropsychological testing and evaluation services. These services are currently on the Medicare Telehealth Services List temporarily for the duration of the PHE. CMS believes that there is likely to be clinical benefit when furnished via telehealth, and therefore, they meet the criteria for temporary inclusion on a Category 3 basis. However, CMS is concerned regarding whether, outside the circumstances of the PHE, the full scope of service elements can occur in a manner that does not jeopardize quality of care, whether this patient population could be fully assessed via interactive audio-video technology, and whether these services could be conducted in a way that maintains the safety of the beneficiary.
- Other Services Proposed for Addition to the Medicare Telehealth Services List
- CMS is proposing to add a number of services to the list on a Category 3 basis that are currently included on the Medicare Telehealth Services List temporarily during the PHE. These services would be included on the Medicare Telehealth Services List through 2023 to allow CMS to evaluate data that may support their permanent addition to the list on a Category 1 or Category 2 basis.
- The services proposed for inclusion to the Medicare Telehealth Services List on a Category 3 basis includes CPT codes 90875, 92012, 92014, 92014, 92507, 94005, 96105, 96110, 96112, 96113, 96127, 96170, 96171, 97129, 97130, and 99473.
- CMS is soliciting comments regarding how widespread the availability of remote audiology testing technology is, and whether interested parties believe these services can be furnished in a way that does not jeopardize patient safety or quality of care when these services are furnished remotely. CMS believes that, in circumstances in which such equipment is available at the originating site, these services can be furnished in a way in which all of the elements of the services are met and that there is likely to be a clinical benefit when these services are furnished via telehealth. Therefore, CMS is proposing to add these services to the Medicare Telehealth Services List on a Category 3 basis, which would allow these services to be available via telehealth through the end of CY 2023.
- CMS is proposing to create codes to describe prolonged services associated with certain types of E/M services. CMS believes these proposed G codes would be sufficiently similar to psychiatric diagnostic procedures or O/O visits currently on the Medicare Telehealth Services List to qualify for inclusion on the list on a Category 1 basis. Therefore, CMS is proposing to add proposed HCPCS codes GXXX1, GXXX2, and GXXX3 to the Medicare Telehealth Services List on a Category 1 basis.
- Table 8 outlines services that CMS is proposing for addition to the Medicare Telehealth Services List on a Category 3 basis. Table 9 lists the services that CMS is proposing for permanent addition to the Medicare Telehealth Services List on a Category 1 basis. See appendix for both tables.
- CMS is proposing to add a number of services to the list on a Category 3 basis that are currently included on the Medicare Telehealth Services List temporarily during the PHE. These services would be included on the Medicare Telehealth Services List through 2023 to allow CMS to evaluate data that may support their permanent addition to the list on a Category 1 or Category 2 basis.
- Services Proposed for Removal from the Medicare Telehealth Services List After 151 Days Following the End of the PHE
- As noted in the CY 2022 PFS final rule (86 FR 65054), at the conclusion of the PHE for COVID-19, the associated waivers and interim policies will expire, payment for Medicare telehealth services will once again be limited by the requirements of section 1834(m) of the Act, and CMS will return to the policies established through the regular notice-and-comment rulemaking process, through which CMS established Medicare Telehealth Services List.
- CMS is proposing to continue to include on the Medicare Telehealth Services List the services that are currently set to be removed from the list when the PHE ends (that is, those not currently added to the list on a Category 1, 2, or 3 basis) for an additional 151 days after the PHE ends. Table 10 (appendix) lists those services that are temporarily available for the PHE, which CMS is proposing to retain on the Medicare Telehealth Services List for an additional 151 days following the end of the PHE. These services will no longer be available on the Medicare Telehealth Services List on the 152nd day after the end of the PHE, payment for Medicare telehealth services will once again be limited by the requirements of section 1834(m) of the Act, as aforementioned, and telehealth claims for these codes will be denied. CMS is proposing to align those services that had been planned to stop being available as Medicare telehealth at the end of the PHE with the 151-day extensions of flexibilities enacted in the CAA, 2022 in order to simplify the process of when flexibilities will end and to minimize possible errors.
- Implementation of Telehealth Provisions of the Consolidation Appropriations Acts, 2021 and 2022
- CMS is proposing to implement provisions of section 1834(m) of the Act (including the amendments made by the CAA, 2021) and provisions of the CAA, 2022 that extend certain Medicare telehealth flexibilities adopted during the PHE for 151 days after the end of the PHE.
- In-Person Requirement for Behavioral Health. Section 304(a) of the CAA, 2022 amended section 1834(m)(7)(B)(i) of the Act to delay the requirement for an in-person visit with a physician or practitioner within six months prior to an initial mental health telehealth service, and again at subsequent intervals as the Secretary determines appropriate. In light of this amendment, the in-person requirements for telehealth services furnished for purposes of diagnosis, evaluation, or treatment of a mental health disorder will again be effective on the 152nd day after the PHE ends. In addition, section 304(b) and (c) of the CAA, 2022 modified sections 1834(y) and 1834(o)(4) of the Act, respectively, to similarly delay in-person visit requirements for mental health visits furnished by Rural Health Clinics and Federally Qualified Health Centers via telecommunications technology.
- Therefore, CMS proposes to update its regulations to recognize the delay of the in-person requirements for mental health visits furnished by RHCs and FQHCs through telecommunication technology under Medicare until the 152nd day after the PHE for COVID-19.
- Audio-Only Telehealth. CMS is proposing to continue to make payment for services included on the Medicare Telehealth Services List as of March 15, 2022 that are furnished via an audio-only telecommunications system for the 151-day period beginning on the first day after the end of the PHE. CMS read section 305 of the CAA, 2022 to require that we continue to make payment for services furnished via audio-only telecommunications systems (each described by a HCPCS code, including their successor codes) for the 151-day period after the end of the PHE. These services include certain behavioral health, counseling, and educational services.
- Given that the end date of the PHE is not yet known and could occur before the rulemaking process for the CY 2023 PFS is complete, and that the changes made by these provisions are very specific and concise, CMS is providing notice that they intend to issue program instructions or other subregulatory guidance to effectuate the changes described above, other than the proposed revisions to § 410.78, in the near future. CMS believes this approach will serve to ensure a smooth transition after the end of the PHE for COVID-19.
- Use of Modifiers for Medicare Telehealth Services Following the End of the PHE for COVID-19
- CMS proposes that Medicare telehealth services furnished on or before the 151st day after the end of the PHE, in alignment with the extensions of telehealth-related flexibilities in the CAA, 2022, will continue to be processed for payment as Medicare telehealth claims when accompanied with the modifier “95”.
- CMS further proposes that physicians and practitioners can continue to report the place of service code that would have been reported had the service been furnished in-person during the 151-day period after the end of the PHE, as finalized on an interim basis in the March 31 IFC (85 FR 19233). Medicare telehealth services performed with dates of service occurring on or after the 152nd day after the end of the PHE will revert to pre-PHE rules and will no longer require modifier “95” to be appended to the claim, but the appropriate place of service (POS) indicator will need to be included on the claim to be processed for payment as Medicare telehealth claims in order to properly identify the place where the service was furnished.
- CMS proposes that, beginning January 1, 2023, a physician or other qualified health care practitioner billing for telehealth services furnished using audio-only communications technology shall append CPT modifier “93” to Medicare telehealth claims (for those services for which the use of audio-only technology is permitted under § 410.78(a)(3)), to identify them as having been furnished using audio-only technology. CMS believes that using modifier “93”, which is a CPT modifier, will simplify billing, as this modifier is used by payers outside of Medicare.
- Other Non-Face-to-Face Services Involving Communications Technology Under the PFS
- Expiration of PHE Flexibilities for Direct Supervision Requirements
- CMS changed the definition of “direct supervision” during the PHE for COVID-19 (85 FR 19245 through 19246) as it pertains to supervision of diagnostic tests, physicians’ services, and some hospital outpatient services, to allow the supervising professional to be immediately available through virtual presence using real-time audio/video technology, instead of requiring their physical presence.
- CMS is seeking information on whether the flexibility to meet the immediate availability requirement for direct supervision through the use of real-time, audio/video technology should potentially be made permanent.
- CMS is seeking comment regarding the possibility of permanently allowing immediate availability for direct supervision through virtual presence using real-time, audio/video technology for only a subset of services, as CMS recognizes that it may be inappropriate to allow direct supervision without physical presence for some services due to potential concerns over patient safety.
- Non-Face-to-Face Services/Remote Therapeutic Monitoring (RTM) Services
- From CY2022 – CMS has heard two concerns related to the clinical labor in the direct PE for the two RTM treatment management codes, CPT codes 98980 and 98981.
- For CY 2023 CMS is proposing to create four new HCPCS G codes with one pair of codes aimed at increasing patient access to remote therapeutic monitoring services and the second pair aimed at reducing physician and NPP supervisory burden.
- CMS considered requests from interested parties to develop a generic device code for RTM and decided to wait to develop a generic RTM device code and instead will seek comment to inform any new coding relating to devices.
- CMS seeks comment about RTM devices that are used to deliver services that meet the “reasonable and necessary” standard under section 1862(a)(1)(A) of the Act.
- CMS seeks information related to the types of data collected using RTM devices, how the data that are collected solve specific health conditions and what those health conditions are, the costs associated with RTM devices that are available to collect RTM data, how long the typical episode of care by condition type might last, and the potential number of beneficiaries for whom an RTM device might be used by the health condition type.
- Proposal to develop two HCPCS G codes that allow certain qualified nonphysician health care professionals to furnish RTM services
- As a means of increasing beneficiary access to RTM services, as well as more clearly defining the services of RTM for qualified nonphysician healthcare practitioners whose Medicare benefit category does not include services provided incident to their own services, CMS is proposing two codes that would expressly facilitate RTM services furnished by qualified nonphysician healthcare professionals who cannot bill under Medicare Part B for services furnished incident to their professional services. These codes would not include “incident to” activities in the practice expense (PE). Neither of the two proposed new codes include clinical labor inputs in the direct PE. CMS is proposing to make the current CPT codes 98980 and 98981 codes non-payable by Medicare.
- Proposed HCPCS G Codes:
- GRTM3 (Remote therapeutic monitoring treatment assessment services, first 20 minutes furnished personally/directly by a nonphysician qualified health care professional over a calendar month requiring at least one interactive communication with the patient/caregiver during the month).
- GRTM4 (Remote therapeutic monitoring treatment assessment services, additional 20 minutes furnished personally/directly by a nonphysician qualified health care professional over a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month (List separately in addition to code for primary procedure))
- CMS is proposing a work RVU of 0.62 for the base code, HCPCS code GRTM3, which is the RUC-recommended work RVU established for CPT code 98980 in the CY 2022 PFS final rule. Similarly, for the add-on code, HCPCS code GRTM4, CMS is proposing a work RVU of 0.61, which is the RUC-recommended value established for CPT code 98981. CMS is proposing to remove the clinical labor inputs in the direct PE for both codes, which will facilitate the use of these codes by qualified nonphysician healthcare practitioners who cannot bill under Medicare Part B for services furnished incident to their professional services. See Table 28: Summary of Proposed HCPCS G Codes for Remote Therapeutic Monitoring Services for more detailed information about the codes.
- All the RTM codes including proposed HCPCS codes GRTM3 and GRTM4 would be designated as “sometimes therapy” codes, which means that the services could be billed outside a therapy plan of care by physicians and certain NPPs. When the services described by proposed HCPCS codes GRTM3 and GRTM4 are furnished by PTs, OTs, or SLPs, the services would always need to be furnished under a therapy plan of care. CMS reminds readers that RTM services that relate to devices specific to therapy services should always be furnished under a therapy plan of care regardless of who provides them. See the Medicare Benefit Policy Manual Chapter 15, Section 230 for more information about the practice of PT, OT, and SLP.
- Proposal to Develop two HCPCS G Codes Allowing General Supervision of Auxiliary Personnel – CMS is proposing to create two HCPCS G codes, one base code and one add-on code, that include clinical labor activities (that is, incident to services such as communicating with the patient, resolving technology concerns, reviewing data, updating and modifying care plans, and addressing lack of patient improvement) that can be furnished by auxiliary personnel under general supervision.
- These two new G codes, GRTM1 and GRTM2, will include physician work and direct PE inputs as currently described in CPT codes 98980 and 98981 but will allow general supervision of the clinical labor found in the direct PE inputs. See Table 28: Summary of Proposed HCPCS G Codes for Remote Therapeutic Monitoring Services for more detailed information about the codes and use of the codes.
- Proposed HCPCS G Codes:
- HCPCS code GRTM1 (Remote therapeutic monitoring treatment management services, physician or NPP professional time over a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; first 20 minutes of evaluation and management services).
- HCPCS code GRTM2 (Remote therapeutic monitoring treatment management services, physician or NPP professional time over a calendar month requiring at least one interactive communication with the patient/caregiver over a calendar month; each additional 20 minutes of evaluation and management services during the calendar month (List separately in additional to code for primary procedure).
- CMS is proposing a work RVU of 0.62 for HCPCS code GRTM1, which reflects the work RVU for CPT code 98980 finalized in the CY 2022 PFS final rule. For HCPCS code GRTM2, CMS is proposing a work RVU of 0.61, which is the RUC-recommended value finalized for the similar CPT code 98981. CMS is proposing the direct PE inputs associated with CPT codes 98980 and 98981 without refinement for HCPCS codes GRTM1 and GRTM2, respectively. CMS is proposing to make the current CPT codes 98980 and 98981 codes non-payable by Medicare.
- Proposed HCPCS G Codes:
- These two new G codes, GRTM1 and GRTM2, will include physician work and direct PE inputs as currently described in CPT codes 98980 and 98981 but will allow general supervision of the clinical labor found in the direct PE inputs. See Table 28: Summary of Proposed HCPCS G Codes for Remote Therapeutic Monitoring Services for more detailed information about the codes and use of the codes.
- Valuation of Specific Codes
(33) Chronic Pain Management and Treatment (CPM) Bundles (HCPCS GYYY1, and GYYY2)
In the CY 2022 PFS proposed rule (86 FR 39104, 39179 – 39181), CMS explored refinements to the PFS that would appropriately value chronic pain management and treatment (CPM) by soliciting comment on CPM for the purpose of future rulemaking. In CMS’ solicitation, they described Federal efforts for more than a decade to effectively address pain management as a response to the nation’s overdose crisis, such as the National Pain Strategy and the HHS Pain Management Best Practices Inter-Agency Task Force (PMTF) Report.
Through solicitation of comments, the CCM/CCCM/PCM code family now includes five sets of codes, each set with a base code and an add-on code. The sets vary by the degree of complexity of care (that is, CCM, CCCM, or PCM), who directly performs the services (that is, clinical staff, or the physician or NPP), and the time spent furnishing the services. The RUC-recommended values for work RVUs and direct PE inputs for these codes in CY 2022 were derived from a recent RUC specialty society survey.
- CMS is seeking comments regarding how best the initial visit and subsequent visits should be conducted (for example, in-person, via telehealth, or the use of a telecommunications system, and any implications for additional or different coding).
- CMS will also consider whether to add the CPM codes to the Medicare Telehealth Services List, based on our review of any information provided through the public comments and CMS analysis of how these new services may be appropriately furnished to Medicare beneficiaries.
- CMS is also asking for comment regarding whether there are components of the proposed CPM services that do not necessarily require face-to-face interaction with the billing practitioner, such as care that could be provided by auxiliary staff incident to the billing practitioner’s services.
(30) Cognitive Behavioral Therapy Monitoring (CPT Code 989X6).
See the Remote Therapeutic Monitoring (RTM) section II.I. of this proposed rule for a review of new device code, CPT code 989X6.
VII. Regulatory Impact Analysis
- Extension of Certain Medicare Telehealth Flexibilities, Under Section 1834(m) of the Act, as Amended by the Consolidated Appropriations Act, 2022
As discussed in section II.D.1.e of this proposed rule, CMS is proposing to implement sections 301, 302, 304, and 305, of the Consolidated Appropriations Act, 2022, which extended the geographic restrictions (section 301), extended the temporary expansion of practitioner types who are eligible to furnish Medicare telehealth (section 302), delayed the in-person requirements under Medicare for mental health services furnished through telehealth under the PFS (section 304), and extended audio-only flexibilities for certain telehealth services that would otherwise not be available via telehealth (section 305) after the expiration of the PHE to remain on the Medicare Telehealth Services List for a 151-day period beginning on the first day after the end of the public health emergency (PHE) for COVID-19.
This proposal is necessary to fulfill the statutory requirement to implement this extension until the 152nd day after the end of the PHE for COVID-19.
- Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs)
As discussed in section III.C.3 of this proposed rule, CMS implements sections 303 and 304 of the Consolidated Appropriations Act, 2022. Section 303 of the CAA, 2022 amended section 1834(m)(8) of the Act to temporarily continue payment for telehealth services furnished by FQHCs and RHCs for the 151-day period beginning on the first day after the end of the COVID-19 PHE using the methodology established for telehealth services furnished by FQHCs and RHCs during the PHE, which, in accordance with section 1834(m)(8)(B) of the Act, is based on payment rates that are similar to the national average payment rates for comparable telehealth services under the PFS.
Section 304 of the CAA, 2022 delays the in-person requirements under Medicare for mental health services furnished through telehealth under the PFS and for mental health visits furnished by RHCs and FQHCs via telecommunications technology for a 151-day period beginning on the first day after the end of the public health emergency (PHE) for COVID-19. These proposals are necessary to fulfill these statutory requirements.
CMS also discusses implementation of sections 301 and 305 of the CAA, 2022 that would apply to telehealth services (those that are not mental health visits) furnished by RHCs and FQHCs. That is, section 301 of the CAA, 2022 extended the geographic restrictions and section 305 of the CAA, 2022 extended audio-only flexibilities for certain telehealth services that would otherwise not be available via telehealth.
Alliance – CY2023 Physician Fee Schedule Proposed Rule – Summary of Telehealth Provisions
Alliance Leads a Letter Supporting the Benefit Expansion for Workers Act of 2022
The Alliance for Connected Care led a letter with other leading telehealth groups supporting the Benefit Expansion for Workers Act of 2022, which would allow employers to provide telehealth or other remote care services to employees ineligible for an employer-sponsored group health plan.
To read the full letter, click here or see below:
 Loading...
Loading...
Alliance Applauds Inclusion of Telehealth Provisions in the FY 2023 House Appropriations Committee Report
On June 29, the House Appropriations Committee released the Report for the Departments of Labor, Health and Human Services, Education, and Related Agencies for Fiscal Year 2023 Appropriations. The report includes specific instructions with respect to the appropriated amounts.
The Alliance was thrilled to see the inclusion of several telehealth provisions in this report, which ensure patients can continue to access care through this modality and data about its usage can be adequately collected to inform future policy. Below is a topline of the key telehealth provisions included in the report language.
HHS Office of the Secretary
- Telehealth Data. —The Committee recognizes that demand for telemedicine increased in 2020 in response to the COVID–19 pandemic. In addition, the Committee notes disparities in telehealth exist between and within racial and ethnic groups, rural and urban locations, and geographic regions as detailed in a December 2021 report by the Assistant Secretary for Planning and Evaluation. The Committee urges the Secretary, working with CMS and HRSA, to categorize telehealth usage data, including for audio-only services, by Health Professional Shortage Areas. The Committee further urges the Secretary to work across agencies to ensure that improvements to broadband availability are prioritized in those areas with lowest telehealth usage, highest audio-only usage, and a known health professional shortage. The Committee requests an update within 120 days of the date of enactment of this Act on this categorization and broadband availability.
Centers for Medicare and Medicaid Services (CMS)
- Telehealth and Health Care Access. —The Committee requests a report in the fiscal year 2024 Congressional Budget Justification on the impact of telehealth on health care access, utilization, cost, and outcomes, broken down by race, ethnicity, sex, age, disability status, and zip code under the Medicaid program and CHIP.
Health Resources and Services Administration (HRSA)
- Telehealth. —The Committee includes $37,050,000 for Telehealth, an increase of $2,000,000 above the fiscal year 2022 enacted level. Funds support the Office for the Advancement of Telehealth, which promotes the effective use of technologies to improve access to health services for people who are isolated from health care and to provide distance education for health professionals.
- Telehealth Provider Bridge. —The Committee includes $500,000 within the total for Telehealth for the Provider Bridge program. With funds appropriated in the Coronavirus License Portability Grant Program, HRSA established the Provider Bridge Program to empower medical professionals to safely and efficiently deliver urgently needed care to communities during public health emergencies. To date, over 400 entities and 85,000 healthcare professionals have leveraged this national tool connecting health care professionals with State agencies and health care entities to quickly verify credentials and professional background information. Specifically, the platform provides a directory of State and Federal COVID–19 resources, allows health care professionals to submit professional background information, produces official and verified digital documents of licensure and credentialing information, and provides access to a database of information for volunteer clinicians willing to provide care.
- Telehealth Centers of Excellence. —The Committee supports the continued development of Telehealth Centers of Excellence to continue to validate technologies and reimbursement mechanisms, establish training protocols, and develop comprehensive templates for States to integrate telehealth into their state health provider networks.
- Rural Telehealth Initiative. —The Committee supports the Memorandum of Understanding entered into on August 31, 2020, establishing a Rural Telehealth Initiative among HHS, the Federal Communications Commission, and the Department of Agriculture. Together, this important initiative can leverage expertise of each respective agency and improve collaboration amongst entities tasked with addressing rural telehealth access. This initiative recognizes the unique problems facing rural Americans that need access to critical care services through telehealth platforms. The Committee encourages agencies involved in this initiative to prioritize opportunities to continue the expansion of telehealth services, close the digital divide, and not leave rural communities behind.
Telehealth Resource Centers Support Letter
On May 31, more than 80 organizations called on Congressional Appropriators to increase funding for Telehealth Resource Centers. This increase in funding would provide a critical boost to the TRCs, which have experienced a high of an 800% increase in demand for telehealth assistance during the COVID-19 pandemic across the nation, yet have been level-funded since 2006. Learn more about this request.
 Loading...
Loading...
 Loading...
Loading...
Spring 2022 Alliance Top Accomplishments
It has already been a momentous year for telehealth. This link and the below PDF provide key highlights of Alliance for Connected Care accomplishments thus far in 2022. We look forward to further successes later this year.
 Loading...
Loading...
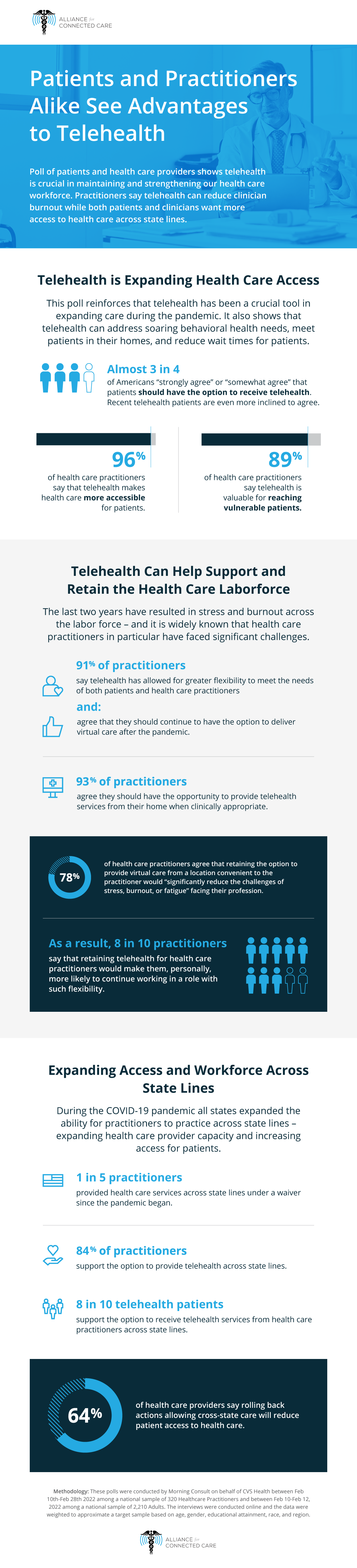
Patients and Practitioners Agree – Telehealth Is Important for Patient Access, Health Care Workforce
Patients and Practitioners Agree – Telehealth Is Important for Patient Access, Health Care Workforce
FOR IMMEDIATE RELEASE
April 6, 2022
WASHINGTON – Today, the Alliance for Connected Care released a major survey of both healthcare patients and practitioners conducted by Morning Consult on the Alliance’s behalf. The poll asked patients and practitioners about their telehealth usage, telehealth experiences, their use of care across state lines, and the workforce implications of these developments.
- A slide deck summarizing the findings can be found here.
- An Alliance infographic of key selected data points can be found here.
- A printable version of the infographic can be found here.
“This is the first time we have polled both patients and providers, and they are aligned on the merits of telehealth,” said Krista Drobac, Executive Director of the Alliance for Connected Care. “I am particularly excited to see practitioners reporting that telehealth is a tool to fight clinical burnout and to see such strong support from patients for access to care across state lines.”
“Effective access to telehealth is essential to improving America’s health care future. The findings of this research reinforce what we have experienced, which is telehealth makes health care easier for patients, and also provides flexibility and opportunities for balance for health care providers, said Brian Hasselfeld, MD, Medical Director, Digital Health and Telemedicine, Johns Hopkins Medicine. “Regulatory and policy changes that preserve these flexibilities, and address barriers such as restrictions on care across state lines, will be important for our patients and health care workforce going forward.”
“Clinicians at Stanford have experienced firsthand the benefits of telehealth for their patients, and we are not surprised to see these results – showing that the overwhelming majority of clinicians and patients support the option to engage in telehealth across state lines,” said Christopher (Topher) Sharp, MD, Chief Medical Information Officer for Stanford Health Care. “Telehealth has been a critical access point, particularly for specialty care which is in such short supply across the US.”
Notable findings of the poll:
The experience with telehealth is positive for both patients and providers
- Almost 3 in 4 of the general population “strongly agree” or “somewhat agree” that patients should have the option to receive telehealth, even after the pandemic. Among recent telehealth patients, this proportion increases to 84%.
- Three quarters of health care providers surveyed say they have provided care via telehealth at least once since the pandemic began. Of those surveyed, 91% of practitioners say telehealth has allowed for greater flexibility to meet the needs of both patients and health care practitioners.
- 91% of health care practitioners also agree that they should continue to have the option to deliver virtual care after the pandemic.
Patients and providers both believe telehealth is increasing access to health care when needed
Telehealth has been a crucial tool to expand the capabilities of the health care system during COVID-19, yet challenges remain. Telehealth may help to address soaring behavioral health needs, meet patients in their homes, and reduce health care wait times for patients. Accordingly –
- 96% of health care practitioners say that telehealth makes health care more accessible for patients.
- 89% of health care practitioners say telehealth is valuable for reaching vulnerable patients.
- 73% of practitioners believe telehealth improves the overall quality of care.
- 66% of adults believe that telehealth will make patients more likely to seek health care when they need it.
- 84% of recent telehealth patients say they have personally benefited from the option to receive care though telehealth.
Both patients and providers support telehealth across state lines
During the COVID-19 pandemic, all 50 states expanded the ability for practitioners to practice across state lines – expanding health care provider capacity and increasing access for patients. Strong support exists for policies to expand opportunities to give and receive care across state lines:
- One in five practitioners surveyed have provided health care services across state lines under a waiver since the pandemic began.
- 84% of health care practitioners support the option to provide telehealth across state lines.
- Over 8 in 10 telehealth patients also support the option to receive telehealth services from health care practitioners across state lines, suggesting that those who have received care via telehealth in the past view their experiences favorably.
- Health care providers expect that state actions to end broad access to care across state lines has had or will have a net negative impact on a variety of indicators:
- 64% say reducing cross-state care will reduce patient access to health care.
- 56% say reducing cross-state care will have a negative effect on health outcomes.
Telehealth is the key to supporting and retaining the health care workforce
Challenges with health care provider burnout are widely reported – and many health care institutions are struggling to recruit and retain the expertise needed to serve patients. Meanwhile – practitioners report that telehealth, and the ability to provide care from a range of locations when clinically appropriate, are a crucial tool to reduce these challenges. The polling found:
- 78% of health care practitioners agree that retaining the option to provide virtual care from a location convenient to the practitioner would “significantly reduce the challenges of stress, burnout, or fatigue” facing their profession.
- As a result, 8 in 10 practitioners say that retaining telehealth for health care practitioners would make them, personally, more likely to continue working in a role with such flexibility.
- 93% of health care practitioners agree they should have the opportunity to provide telehealth services from their home when clinically appropriate.
- 79% of health care practitioners and 84% of telehealth patients support allowing nurse practitioners to provide care to the full extent of their education and licensure, including through telehealth.
These findings have far-ranging implications for policymakers at both the state and federal levels. The Alliance for Connected Care looks forward to working with policymakers in these endeavors to improve the health and well being of all Americans.
Alliance submits comments in response to the White House Office of Science and Technology Policy on Strengthening Community Health Through Technology RFI
The Alliance for Connected Care submitted comments in response to the request for information from the White House Office of Science and Technology Policy (OSTP) on strengthening community health through technology.
The Alliance specifically commented on the burdensome licensure requirements which create a barrier in access to virtual health care. The Alliance recommends the federal government to:
- Develop and implement a national framework for interstate licensure; and
- Address state licensing limitations that impact clinical trial recruitment and diversity.
The Alliance believes telehealth and remote patient monitoring are important tools for bringing innovative services and treatments to those with the least access to it, however there continue to be barriers in place that impede such access. Provider shortages are associated with delayed health care usage, reduced continuity of care, higher health care costs, worse prognoses, less adherence to care plans, and increased travel. State lines create artificial barriers to the delivery of care – complicating access for patients and creating additional burden on clinicians.
To read the full letter, click here or see below:
 Loading...
Loading...
Effectiveness of Remotely Delivered Interventions to Simultaneously Optimize Management of Hypertension, Hyperglycemia and Dyslipidemia in People With Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Frontiers in Endocrinology: Effectiveness of Remotely Delivered Interventions to Simultaneously Optimize Management of Hypertension, Hyperglycemia and Dyslipidemia in People With Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Background: Remotely delivered interventions may be more efficient in controlling multiple risk factors in people with diabetes.
Purpose: To pool evidence from randomized controlled trials testing remote management interventions to simultaneously control blood pressure, blood glucose and lipids.
Data Sources: PubMed/Medline, EMBASE, CINAHL and the Cochrane library were systematically searched for randomized controlled trials (RCTs) until 20th June 2021.
Study Selection: Included RCTs were those that reported participant data on blood pressure, blood glucose, and lipid outcomes in response to a remotely delivered intervention.
Data Extraction: Three authors extracted data using a predefined template. Primary outcomes were glycated hemoglobin (HbA1c), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-c), systolic and diastolic blood pressure (SBP & DBP). Risk of bias was assessed using the Cochrane collaboration RoB-2 tool. Meta-analyses are reported as standardized mean difference (SMD) with 95% confidence intervals (95%CI).
Data Synthesis: Twenty-seven RCTs reporting on 9100 participants (4581 intervention and 4519 usual care) were included. Components of the remote management interventions tested were identified as patient education, risk factor monitoring, coaching on monitoring, consultations, and pharmacological management. Comparator groups were typically face-to-face usual patient care. Remote management significantly reduced HbA1c (SMD -0.25, 95%CI -0.33 to -0.17, p<0.001), TC (SMD -0.17, 95%CI -0.29 to -0.04, p<0.0001), LDL-c (SMD -0.11, 95%CI -0.19 to -0.03, p=0.006), SBP (SMD -0.11, 95%CI -0.18 to -0.04, p=0.001) and DBP (SMD -0.09, 95%CI -0.16 to -0.02, p=0.02), with low to moderate heterogeneity (I²= 0 to 75). Twelve trials had high risk of bias, 12 had some risk and three were at low risk of bias.
Limitations: Heterogeneity and potential publication bias may limit applicability of findings.
Conclusions: Remote management significantly improves control of modifiable risk factors.
Alliance submits comments in response to Healthy Future Task Force Treatments Subcommittee RFI
The Alliance for Connected Care submitted comments in response to the request for information from the Treatments Subcommittee of the Healthy Future Task Force regarding medical innovation to supercharge the availability and development of life-saving treatments, devices, and diagnostics, while addressing rising costs to patients.
The Alliance specifically commented on the question under “Goal 4: Increase access to medical innovation” about decentralizing clinical trials in order to expand access to innovative treatments to patients through remote monitoring.
The Alliance believes continuing to modernize and decentralize clinical trials is critical for creating opportunities for more diversity and patient engagement. Obviating the need for travel time, lost wages and childcare/eldercare through use of digital technologies will significantly increase the pool of potential participants in clinical trials across geographies. However, state licensing limitations continue to present a barrier to decentralizing clinical trials, and effectively prohibit clinicians working on clinical trials from recruiting patients from outside the state where the clinician is licensed.
To read the full letter, click here or see below:
 Loading...
Loading...