Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial
Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial
Background: There is a paucity of evidence for dose and pace of up-titration of guideline-directed medical therapies after admission to hospital for acute heart failure.
Methods: In this multinational, open-label, randomised, parallel-group trial (STRONG-HF), patients aged 18-85 years admitted to hospital with acute heart failure, not treated with full doses of guideline-directed drug treatment, were recruited from 87 hospitals in 14 countries. Before discharge, eligible patients were randomly assigned (1:1), stratified by left ventricular ejection fraction (≤40% vs >40%) and country, with blocks of size 30 within strata and randomly ordered sub-blocks of 2, 4, and 6, to either usual care or high-intensity care. Usual care followed usual local practice, and high-intensity care involved the up-titration of treatments to 100% of recommended doses within 2 weeks of discharge and four scheduled outpatient visits over the 2 months after discharge that closely monitored clinical status, laboratory values, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) concentrations. The primary endpoint was 180-day readmission to hospital due to heart failure or all-cause death. Efficacy and safety were assessed in the intention-to-treat (ITT) population (ie, all patients validly randomly assigned to treatment). The primary endpoint was assessed in all patients enrolled at hospitals that followed up patients to day 180. Because of a protocol amendment to the primary endpoint, the results of patients enrolled on or before this amendment were down-weighted. This study is registered with ClinicalTrials.gov, NCT03412201, and is now complete.
Findings: Between May 10, 2018, and Sept 23, 2022, 1641 patients were screened and 1078 were successfully randomly assigned to high-intensity care (n=542) or usual care (n=536; ITT population). Mean age was 63·0 years (SD 13·6), 416 (39%) of 1078 patients were female, 662 (61%) were male, 832 (77%) were White or Caucasian, 230 (21%) were Black, 12 (1%) were other races, one (<1%) was Native American, and one (<1%) was Pacific Islander (two [<1%] had missing data on race). The study was stopped early per the data and safety monitoring board’s recommendation because of greater than expected between-group differences. As of data cutoff (Oct 13, 2022), by day 90, a higher proportion of patients in the high-intensity care group had been up-titrated to full doses of prescribed drugs (renin-angiotensin blockers 278 [55%] of 505 vs 11 [2%] of 497; β blockers 249 [49%] vs 20 [4%]; and mineralocorticoid receptor antagonists 423 [84%] vs 231 [46%]). By day 90, blood pressure, pulse, New York Heart Association class, bodyweight, and NT-proBNP concentration had decreased more in the high-intensity care group than in the usual care group. Heart failure readmission or all-cause death up to day 180 occurred in 74 (15·2% down-weighted adjusted Kaplan-Meier estimate) of 506 patients in the high-intensity care group and 109 (23·3%) of 502 patients in the usual care group (adjusted risk difference 8·1% [95% CI 2·9-13·2]; p=0·0021; risk ratio 0·66 [95% CI 0·50-0·86]). More adverse events by 90 days occurred in the high-intensity care group (223 [41%] of 542) than in the usual care group (158 [29%] of 536) but similar incidences of serious adverse events (88 [16%] vs 92 [17%]) and fatal adverse events (25 [5%] vs 32 [6%]) were reported in each group.
Interpretation: An intensive treatment strategy of rapid up-titration of guideline-directed medication and close follow-up after an acute heart failure admission was readily accepted by patients because it reduced symptoms, improved quality of life, and reduced the risk of 180-day all-cause death or heart failure readmission compared with usual care.
Alliance Statement on Pandemic Response Accountability Committee Report on Telehealth Use and Program Integrity Risks During COVID-19
Share:
On December 1, 2022, the Pandemic Response Accountability Committee issued a report on telehealth use and program integrity risks across selected health care programs during the first year of the COVID-19 pandemic. Given the debate on Capitol Hill about the permanent flexibilities in the Medicare program, we focus here on Medicare fee-for-service and Medicare Advantage, which HHS examined from March 2020 through February 2021, and the year prior from March 2019 through February 2020.
The report shared several impressive findings:
- 37 million individuals used telehealth services across the programs of six federal agencies – an expansion from approximately 3 million individuals using telehealth in the prior year. Pre-pandemic, the vast majority of those telehealth visits were only available to veterans.
- In Medicare, the expansion was huge – with over 80 times the number of individuals using telehealth in 2020.
The report identifies some potential areas of program integrity concern. While there will always be program integrity risks in federal programs, we urge policymakers to keep it in perspective. There is no evidence of a need for widespread concern related to telehealth in the Medicare program. In fact, the telehealth risks appear lower than in-person care.
HHS OIG Claim: “In total, Medicare paid over $5.1 billion for telehealth services for beneficiaries enrolled in Medicare fee-for-service. HHS OIG identified more than 300 Medicare providers who billed for telehealth services at the highest, most expensive level every time, totaling approximately $5.2 million.”
- Perspective:
- The report identified 300 Medicare providers who billed for telehealth services at the highest, most expensive level every time was 0.1 percent of total Medicare payment for telehealth services for beneficiaries enrolled in Medicare fee-for-service. For 2020, Medicare spending was $829.5 billion for total Medicare services.
- As context, the estimated Medicare total improper payment rate in 2020 was 6.27 percent, representing $25.74 billion in improper payments. Prior to the pandemic, the Medicare improper payment rate in 2019 was 25 percent. Other government watchdogs estimated $43 billion in FY 2020 for Medicare improper payments, accounting for over one-quarter of the total amount of improper payments made government-wide in fiscal year 2019.
HHS OIG Claim: “We identified over 1,700 providers whose billing for telehealth services poses a high risk to Medicare. Although these providers represent a small proportion of the approximately 742,000 providers who billed for a telehealth service, their billing raises concern.”
- Perspective: An identification of providers who pose a high risk to Medicare does not indicate the presence of fraud – only that there are practices which should be monitored.
- This point made by HHS OIG is out of context. OIG originally mentioned these providers in this report where they noted that more than half of those high-risk providers belonged to a medical practice that posed high risk billing to Medicare in general, not just telehealth. As such, the billing practices of these providers do not pose a risk solely as it relates to telehealth – they are risks to the Medicare program broadly that CMS should address.
HHS OIG Claim: “HHS OIG identified 138 providers who repeatedly billed both Medicare fee-for-service and a Medicare Advantage plan for the same telehealth service.”
- Perspective: There are bad actors within the Medicare program, 138 providers is a low number for such billing practices to be occurring for the 28 million Medicare beneficiaries who used telehealth services and the $5.1 billion in spending on Medicare telehealth services during the first year of the pandemic.
- In its September 2022 report on program integrity risks in Medicare telehealth services during the first year of the pandemic, HHS OIG noted that a total of 18,034 providers billed both Medicare fee-for-service and Medicare Advantage for the same telehealth service for the same beneficiary on the same date of service at least once. However, HHS OIG only classified providers as “high risk” if they billed this way for more than 20 percent of their claims and encounters – in this case 0.7 percent of providers who billed this way.
- While OIG claims this could be an indicator of providers intentionally submitting duplicate claims to increase their Medicare payments, there is no concrete evidence to support this claim, nor is there an indication of the circumstances surrounding these claims (i.e., potential for practitioner error).
- In 2018, OIG found that many of the disallowed payments for telehealth services were because of practitioner errors in understanding and meeting Medicare telehealth requirements. One of their recommendations was to offer education and training sessions to practitioners on Medicare telehealth requirements. Given that this was the case for the limited number of practitioners using telehealth in 2018, we have a hard time believing there were not many similar errors in 2020.
HHS OIG Claim: “HHS OIG identified 86 providers who billed for a high average number of hours of telehealth services per visit.”
- Perspective: This again is a low number compared to the patients served and spending that occurred, and could be related to any number of factors such as practitioner error in codes used, the nature of the service rendered, or treatment of high-need patients.
- In the same September 2022 report mentioned above, HHS OIG identified 86 providers that billed for an average of more than two hours of telehealth services per visit, compared to the median of 21 minutes of telehealth services per visit for all providers who billed for telehealth services. However, OIG does not note the types of services rendered for these longer visits, which is a critical data point necessary to make accurate comparisons to affirm whether there is call for widespread concern.
- A visit with a psychotherapist who is treating a patient in crisis for a mental health or substance use disorder, for example, is going to require more intensive time and care compared to a visit for acute conditions. HHS OIG notes in a previous report that, during the first year of the pandemic, “beneficiaries used telehealth for 43 percent of behavioral health services, whereas they used telehealth for 13 percent of office visits.” Given the proliferation of telehealth for mental and behavioral health services in particular during the pandemic, this merits further analysis.
It’s important to note that this report recycles past policy recommendations made by HHS OIG. These recommendations include:
- Strengthen monitoring and targeted oversight of telehealth services;
- The Alliance has supported additional oversight to ensure bad actors do not undermine access to telehealth in Medicare.
- Provide additional education to providers on appropriate billing for telehealth services;
- The Alliance strongly agrees that provider education is useful, as accidental misbilling has in the past been interpreted as fraudulent. Similarly, HHS steps to simplify telehealth billing are welcomed.
- Improve the transparency of “incident to” services when clinical staff primarily delivered a telehealth service;
- The Alliance recognizes the importance of accurate data for analysis. We also stress the importance maintaining “incident to” services for healthcare practitioners unable to bill the Medicare program directly.
- Identify telehealth companies that bill Medicare;
- If a provider, including a virtual-only provider, wants to bill Medicare directly, they must enroll in Medicare, thereby giving CMS oversight of that provider. We don’t believe there is clear justification for singling out virtual-only providers, particularly when Medicare beneficiaries are overwhelmingly seeing providers that use telehealth services in addition to maintaining brick and mortar. Given that virtual-only is a new modality, limited steps to improve CMS’s understanding and oversight of these providers seems logical, and if it helps prevent limits on beneficiary access to telehealth, then we support it.
- Require a modifier to identify all audio-only telehealth services provided in Medicare; and
- HHS has already acted on this recommendation, with Alliance for Connected Care support.
- Collect data on the use of telehealth in opioid treatment programs.
- The Alliance recognizes the importance of accurate data for analysis and supports calls for additional data to further analyze this occurrence.
 Loading...
Loading...
Telehealth Expansion: What Does the Data Show?
Thanks to those who were able to join the Alliance for Connected Care and Healthcare Leadership Council for the Telehealth Expansion: What Does the Data Show webinar on November 17, 2022.
The Alliance for Connected Care and the Healthcare Leadership Council held a virtual discussion about telehealth data on November 17, 2022. Attendees heard from experts who discussed the implications of both their own and national telehealth data on our understanding of health care utilization, quality, and access.
The discussion on telehealth data supports the Alliance for Connected Care’s commissioned analysis on Medicare telehealth, which found no evidence that telehealth added to the total volume of Medicare services, and no evidence that patients initiating care who use telehealth had more E&M revisits for the same medical issue than patients with in-person visits.
Of significant note with respect to Medicare spending, the average per service cost of an E&M telehealth visit to the Medicare program is less than in-person services by approximately 20 percent. The reason for this difference was that telehealth clinicians generally billed shorted visit codes than in-person providers.
Find the slides from the webinar below or here.
 Loading...
Loading...
See notable telehealth research below or here.
 Loading...
Loading...
More information about the studies discussed at the webinar:
Alliance Signs Letter Urging Congress to Extend HDHP Telehealth Flexibilities
On November 15, 2022, the Alliance for Connected Care and more than 350 organizations signed a letter urging Congress to extend the telehealth provision that allows employers the flexibility to offer telehealth services pre-deductible to employees with a high deductible health plan coupled with a Health Savings Account (HDHP-HSA). The letter reminds congressional leaders that without legislative action, employers will be required to charge employees more to access telehealth services, creating a barrier to care, including telemental health.
Without action by Congress, this provision will expire on December 31, 2022. New action is needed to ensure Americans do not lose access to these important telehealth benefits again come 2023.
To read the letter, see below or click here.
 Loading...
Loading...
Alliance and Others Send Letter to DEA to Advance Proposed Rules on the Special Registration Telemedicine
Alliance and Others Send Letter to DEA to Advance Proposed Rules on the Special Registration Telemedicine
The Alliance for Connected Care and more than 300 participants sent a letter urging the DEA to advance the proposed rules on the Special Registration for Telemedicine under the Ryan Haight Act to the Office of Management and Budget (OMB). The proposed rule would enable a practitioner to deliver, distribute, dispense, or prescribe via telemedicine a controlled substance to a patient who has not been medically examined in-person by the prescribing practitioner. Without immediate action, there will be a gap between the finalization of the proposed rule and the imminent expiration of the COVID-19 public health emergency (PHE) flexibilities.
Read the full letter here and below:
 Loading...
Loading...
Results of a Remotely Delivered Hypertension and Lipid Program in More Than 10 000 Patients Across a Diverse Health Care Network
Results of a Remotely Delivered Hypertension and Lipid Program in More Than 10 000 Patients Across a Diverse Health Care Network
Importance Blood pressure (BP) and cholesterol control remain challenging. Remote care can deliver more effective care outside of traditional clinician-patient settings but scaling and ensuring access to care among diverse populations remains elusive.
Objective To implement and evaluate a remote hypertension and cholesterol management program across a diverse health care network.
Design, Setting, and Participants Between January 2018 and July 2021, 20 454 patients in a large integrated health network were screened; 18 444 were approached, and 10 803 were enrolled in a comprehensive remote hypertension and cholesterol program (3658 patients with hypertension, 8103 patients with cholesterol, and 958 patients with both). A total of 1266 patients requested education only without medication titration. Enrolled patients received education, home BP device integration, and medication titration. Nonlicensed navigators and pharmacists, supported by cardiovascular clinicians, coordinated care using standardized algorithms, task management and automation software, and omnichannel communication. BP and laboratory test results were actively monitored.
Main Outcomes and Measures Changes in BP and low-density lipoprotein cholesterol (LDL-C).
Results The mean (SD) age among 10 803 patients was 65 (11.4) years; 6009 participants (56%) were female; 1321 (12%) identified as Black, 1190 (11%) as Hispanic, 7758 (72%) as White, and 1727 (16%) as another or multiple races (including American Indian or Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, unknown, other, and declined to respond; consolidated owing to small numbers); and 142 (11%) reported a preferred language other than English. A total of 424 482 BP readings and 139 263 laboratory reports were collected. In the hypertension program, the mean (SD) office BP prior to enrollment was 150/83 (18/10) mm Hg, and the mean (SD) home BP was 145/83 (20/12) mm Hg. For those engaged in remote medication management, the mean (SD) clinic BP 6 and 12 months after enrollment decreased by 8.7/3.8 (21.4/12.4) and 9.7/5.2 (22.2/12.6) mm Hg, respectively. In the education-only cohort, BP changed by a mean (SD) −1.5/−0.7 (23.0/11.1) and by +0.2/−1.9 (30.3/11.2) mm Hg, respectively (P < .001 for between cohort difference). In the lipids program, patients in remote medication management experienced a reduction in LDL-C by a mean (SD) 35.4 (43.1) and 37.5 (43.9) mg/dL at 6 and 12 months, respectively, while the education-only cohort experienced a mean (SD) reduction in LDL-C of 9.3 (34.3) and 10.2 (35.5) mg/dL at 6 and 12 months, respectively (P < .001). Similar rates of enrollment and reductions in BP and lipids were observed across different racial, ethnic, and primary language groups.
Conclusions and Relevance The results of this study indicate that a standardized remote BP and cholesterol management program may help optimize guideline-directed therapy at scale, reduce cardiovascular risk, and minimize the need for in-person visits among diverse populations.
Key Telehealth Provisions in the Calendar Year 2023 Physician Fee Schedule Final Rule
Share:
On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) issued the Calendar Year (CY) 2023 Physician Fee Schedule (PFS) final rule. The rule updates payment rates and finalize policy changes effective January 1, 2023. See the Press Release, Fact Sheet, Fact Sheet (MSSP), and the Final Rule.
General
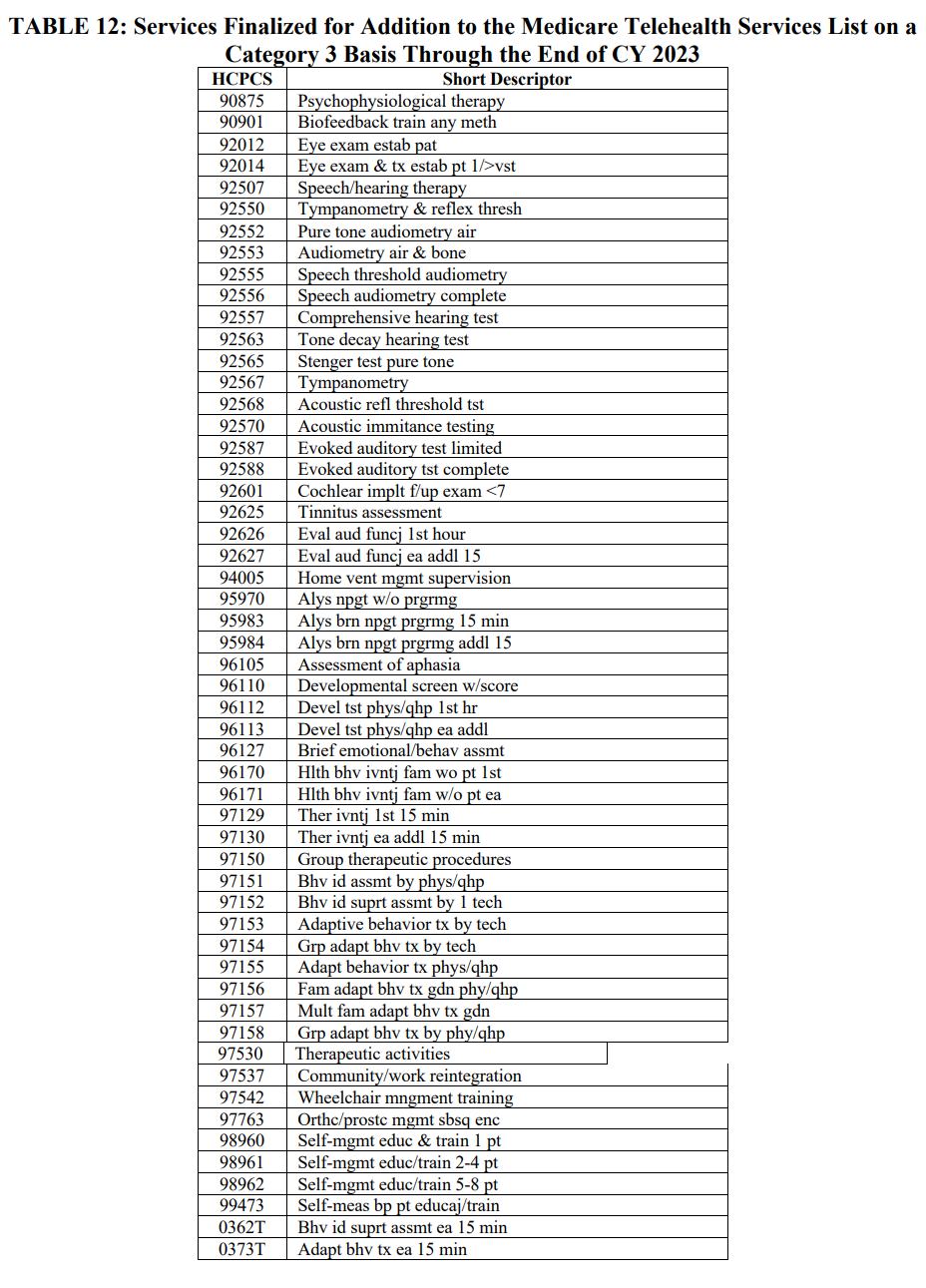
CMS finalized its proposal to add some services to the Medicare Telehealth Services List on a Category 3 basis through the end of 2023, some of which had not been previously added to the Medicare Telehealth List during the PHE, but will be added on a sub regulatory basis.
In addition, CMS finalized its proposal that Medicare telehealth services furnished on or before the 151st day after the end of the PHE, in alignment with the extensions of telehealth-related flexibilities in the CAA, 2022, will continue to be processed for payment as Medicare telehealth claims when accompanied with the modifier “95”. CMS also finalized its proposal that physicians and practitioners can continue to report the place of service code that would have been reported had the service been furnished in-person during the 151-day period after the end of the PHE, as finalized on an interim basis in the March 31 IFC.
Payment for Medicare Telehealth Services Under Section 1834(m) of the Act
Requests to Add Services to the Medicare Telehealth Services List for CY 2023
CMS found that none of the requests received by the February 10 submission deadline met Category 1 or Category 2 criteria for permanent addition to the Medicare telehealth services list. As a reminder, Category 1 are services that are similar to professional consultations, office visits, and office psychiatry services that are currently on the Medicare Telehealth Services list, and the criterion for adding services under Category 2 is that there is evidence of clinical benefit if provided as telehealth.
CMS also assessed the appropriateness of adding the proposed services to the Medicare Telehealth Services List on a Category 3 basis instead. CMS did not propose changes to the length of time the services included on the temporary Category 3 basis. Category 3 will continue to be included through the end of CY 2023. In the event the public health emergency (PHE) extends into CY 2023, CMS may consider revising this policy.
After consideration of public comments, CMS is finalizing the proposed addition of CPT codes 90901, 97150, 97530, 97537, 97542, 97763, and 98960-98962 to the Medicare Telehealth Services List on a Category 3 basis through the end of CY 2023. CMS believes their proposal, consistent with the amendments made by provisions of the CAA, 2022, to extend the period that these services will be available on the Medicare Telehealth Services List temporarily for the PHE by 151 days following the end of the PHE will further enhance the opportunity for the collection of information on the experiences of clinicians who are furnishing telehealth services during the PHE for COVID–19. This will also help CMS to determine which services may ultimately be eligible for permanent addition under Category 1 or Category 2 criteria. CMS encourages interested parties to use this extended time period to gather data on use of services, that is more than statements of support and more than subjective attestations of clinical benefit, to support their potential addition in future rulemaking.
CMS did not finalize its proposal to keep telephone E/M services on the Medicare Telehealth Services List after the end of the PHE and the 151-day post-PHE extension period. CMS believes the statute requires that telehealth services be so analogous to in-person care such that the telehealth service is essentially a substitute for a face-to-face encounter. CMS does not believe that, outside of the circumstances of the PHE, the telephone E/M services would be analogous to in-person care; nor would they be a substitute for a face-to-face encounter. While CMS acknowledges that audio-only technology can be used to furnish mental health telehealth services to patients in their homes under certain circumstances after the PHE ends, two-way, audio-video communications technology continues to be the appropriate standard that will apply for Medicare telehealth services after the PHE and the 151-day extension period. At the conclusion of the PHE and the 151-day extension period provided by the CAA, 2022, the only Medicare telehealth services that will be permitted to be furnished using audio-only technology will be the mental health telehealth services. When a practitioner furnishes such an E/M service using audio-only technology, they would bill for the same service they would bill if the service had been furnished in person. As such, there is not a need to add the telephone-only E/M codes to the Medicare Telehealth Services List for this purpose.
CMS did not finalize its proposal to add GI Tract Imaging, CPT code 91110 and Ambulatory Continuous Glucose Monitoring, CPT code 95251 services to the Medicare Telehealth Services List on a Category 3 basis. CMS does not believe these CPT codes describe services that are a substitute for an in-person visit, and the services that are not inherently face-to-face services are not services that can be furnished as Medicare telehealth services.
CMS finalized its proposal to add CPT codes 95970, 95983, and 95984 to the Medicare Telehealth Services List on a Category 3 basis. Medicare claims data suggest that these services are being provided via telehealth and CMS believes there is some possible clinical benefit for these services when furnished via telehealth; however, there is not yet sufficient evidence available to consider the services for permanent addition to the Medicare Telehealth Services List under the Category 1 or Category 2 criteria.
CMS finalized its proposal to retain emotional/behavior assessment, psychological, or neuropsychological testing and evaluation services on the Medicare Telehealth Services List on a Category 3 basis. CMS believes more time may be necessary to develop evidence that could support the decision to add these services to the Medicare Telehealth Services List permanently on a Category 1 or Category 2 basis.
Other Services Proposed for Addition to the Medicare Telehealth Services List
CMS finalized its proposal to add a number of services to the list on a Category 3 basis that are currently included on the Medicare Telehealth Services List temporarily during the PHE. These services would be included on the Medicare Telehealth Services List through 2023 to allow us to evaluate data that may support their permanent addition to the list on a Category 1 or Category 2 basis.
- The services added to the Medicare Telehealth Services List on a Category 3 basis includes CPT codes 90875, 92012, 92014, 92014, 92507, 94005, 96105, 96110, 96112, 96113, 96127, 96170, 96171, 97129, 97130, and 99473. (See table above)
CMS finalized its proposal to add the remote audiology testing services to the Medicare Telehealth Services List on a Category 3 basis, which would allow these services to be available via telehealth through the end of CY 2023.
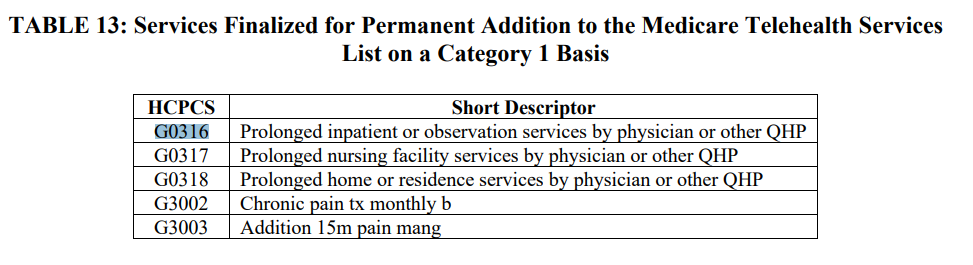
CMS finalized its proposal to create HCPCS codes G0316, G0317, G0318 to the Medicare Telehealth Services List on a Category 1 basis. These codes will be replacing existing codes that describe prolonged services, specifically inpatient prolonged services CPT codes 99356 and 99357.
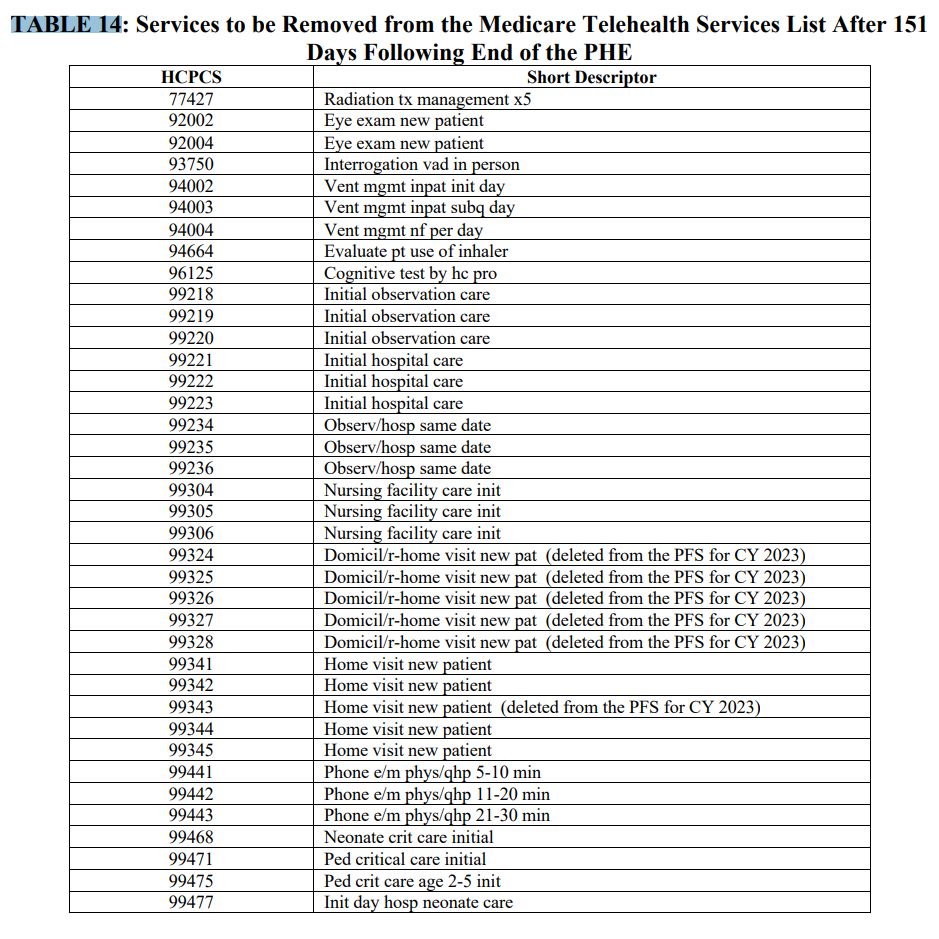
Services Proposed for Removal from the Medicare Telehealth Services List After 151 Days Following the End of the PHE
As noted in the CY 2022 PFS final rule (86 FR 65054), at the conclusion of the PHE for COVID-19, the associated waivers and interim policies will expire, payment for Medicare telehealth services will once again be limited by the requirements of section 1834(m) of the Act, and CMS will return to the policies established through the regular notice-and-comment rulemaking process, through which CMS established Medicare Telehealth Services List.
CMS finalized its proposal to continue to include on the Medicare Telehealth Services List the services that are currently set to be removed from the list when the PHE ends (that is, those not currently added to the list on a Category 1, 2, or 3 basis) for an additional 151 days after the PHE ends.
Implementation of Telehealth Provisions of the Consolidation Appropriations Acts, 2021 and 2022
CMS finalized policies to implement provisions of section 1834(m) of the Act (including the amendments made by the CAA, 2021) and provisions of the CAA, 2022 that extend certain Medicare telehealth flexibilities adopted during the PHE for 151 days after the end of the PHE, including originating site, practitioner type, in-person visit requirements on mental health, and other congressionally extended authorities.
Use of Modifiers for Medicare Telehealth Services Following the End of the PHE for COVID-19
CMS finalized its proposal that Medicare telehealth services furnished on or before the 151st day after the end of the PHE, in alignment with the extensions of telehealth-related flexibilities in the CAA, 2022, will continue to be processed for payment as Medicare telehealth claims when accompanied with the modifier “95”. Practitioners will continue to bill with modifier 95 along with the POS code corresponding to where the service would have been furnished in-person through the later of the end of the year in which the PHE ends or CY 2023.
CMS finalized its proposal that, beginning January 1, 2023, a physician or other qualified health care practitioner billing for telehealth services furnished using audio-only communications technology shall append CPT modifier “93” to Medicare telehealth claims (for those services for which the use of audio-only technology is permitted under § 410.78(a)(3)), to identify them as having been furnished using audio-only technology. CMS believes that using modifier “93”, which is a CPT modifier, will simplify billing, as this modifier is used by payers outside of Medicare.
CMS is also finalizing its proposal to require all providers including RHCs, FQHCs, and OTPs to use modifier “93” when billing for eligible mental health services furnished via audio-only telecommunications technology. Providers have the option to use the “FQ” or the 93” modifiers or both where appropriate and true, since they are identical in meaning. Supervising practitioners continue to be required to append the “FR” modifier on any applicable telehealth claim when they provide direct supervision for a service using virtual presence through real-time, audio and video telecommunications technology.
Other Non-Face-to-Face Services Involving Communications Technology Under the PFS
Expiration of PHE Flexibilities for Direct Supervision Requirements
CMS changed the definition of “direct supervision” during the PHE for COVID-19 as it pertains to supervision of diagnostic tests, physicians’ services, and some hospital outpatient services, to allow the supervising professional to be immediately available through virtual presence using real-time audio/video technology, instead of requiring their physical presence.
CMS sought comment on whether the flexibility to meet the immediate availability requirement for direct supervision through the use of real-time, audio/video technology should potentially be made permanent, and on the possibility of permanently allowing immediate availability for direct supervision through virtual presence using real-time, audio/video technology for only a subset of services.
In the final rule, CMS notes that it plans to continue to gather information on this topic. CMS believes allowing additional time to collect information and evidence for direct supervision through virtual presence will help CMS to better understand the potential circumstances in which this flexibility could be appropriate permanently, outside of the PHE for COVID-19. CMS expects to continue to permit direct supervision through virtual presence through at least the end of CY 2023.
Telehealth Facility Payment Rate
CMS has abandoned its proposal to pay telehealth at the facility rate following the 151-day period. It is instead finalizing a proposal to continue to allow for payment be made for Medicare telehealth services at the rate that ordinarily would have been paid under the PFS if the services were furnished in-person, through the latter of the end of the of CY 2023 or the end of the calendar year in which the PHE ends. For those services furnished in a facility as an originating site, POS 02 may be used, and the corresponding facility fee can be billed, per pre-PHE policy, beginning the 152nd day after the end of the PHE. CMS is concerned about issues raised by commenters related to payment stability in the post-PHE period as care delivery will potentially be transitioning between virtual, hybrid, and in-person models.
Telehealth Originating Site Facility Fee Update
For CY 2023, the final payment amount for HCPCS code Q3014 (Telehealth originating site facility fee) is $28.64. The CY2022 rate was $27.59
Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs)
CMS finalized the proposal to implement sections 303 and 304 of the Consolidated Appropriations Act, 2022 to:
- Temporarily continue payment for telehealth services furnished by FQHCs and RHCs for the 151-day period beginning on the first day after the end of the COVID-19 PHE using the methodology established for telehealth services furnished by FQHCs and RHCs during the PHE, which is based on payment rates that are similar to the national average payment rates for comparable telehealth services under the PFS.
- Delay the in-person requirements under Medicare for mental health services furnished through telehealth under the PFS and for mental health visits furnished by RHCs and FQHCs via telecommunications technology for a 151-day period beginning on the first day after the end of the public health emergency (PHE) for COVID-19. These proposals are necessary to fulfill these statutory requirements.
Remote Therapeutic Monitoring Services
CMS is not finalizing the proposal to create 4 new G-codes, (GRTM-1-4) which were proposed to address various issues relating to incident-to services, inclusions of clinical staff time, and supervision levels. CMS agreed that confusion remains about how the new G-codes, if finalized, would or would not possibly create a chilling effect on the availability of RTM services. CMS will continue to gather information and consider the need for further rulemaking regarding these services.
Instead, the rule, includes a clarification and new policy regarding the billing requirements for the current RTM codes: CPT codes 98975, 98976, 98977, 98980, and 98981. Beginning January 1, 2023, below modifications to our existing RTM policies take effect:
- General supervision for all RTM services- Any RTM service may be furnished under general supervision requirements.
- Cognitive behavioral therapy monitoring device – CMS is finalizing the proposal to accept the RUC recommendation to contractor price CPT code 989X6, a PE-only device code.
Behavioral Health
Tele-behavioral health
In-Person Requirement
Section 304(a) of the CAA, 2022 amended section 1834(m)(7)(B)(i) of the Act to delay the requirement for an in-person visit with a physician or practitioner within 6 months prior to an initial mental health telehealth service, and again at subsequent intervals as the Secretary determines appropriate. In light of this amendment, the in-person requirements for telehealth services furnished for purposes of diagnosis, evaluation, or treatment of a mental health disorder will again be effective on the 152nd day after the PHE ends. In addition, section 304(b) and (c) of the CAA, 2022 modified sections 1834(y) and 1834(o)(4) of the Act, respectively, to similarly delay in-person visit requirements for mental health visits furnished by Rural Health Clinics and Federally Qualified Health Centers via telecommunications technology.
CMS clarifies in the final rule that CMS does not believe the in-person requirement applies to beneficiaries who began receiving mental health telehealth services in their homes during the PHE. In other words, if a beneficiary began receiving mental health telehealth services during the PHE or during the 151-day period after the end of the PHE, then they would not be required to have an in-person visit within 6 months; rather, they will be considered established and will instead be required to have at least one in-person visit every 12 months (so long as any such subsequent telehealth service is furnished by the same individual physician or practitioner (or a practitioner of the same sub-specialty in the same practice) to the same beneficiary). This means that these services would be subject to the requirement that an in-person visit is furnished within 12 months of each mental health telehealth service for those services that are subject to in-person visit requirements (unless an exception is documented by their treating practitioner).
Chronic Pain Management and Treatment (CPM) Bundles (HCPCS GYYY1, and GYYY2)
In the CY 2022 PFS proposed rule (86 FR 39104, 39179 – 39181), CMS explored refinements to the PFS that would appropriately value chronic pain management and treatment (CPM) by soliciting comment on CPM for the purpose of future rulemaking. In CMS’s solicitation, they described Federal efforts for more than a decade to effectively address pain management as a response to the nation’s overdose crisis, such as the National Pain Strategy and the HHS Pain Management Best Practices Inter-Agency Task Force Report.
Through solicitation of comments, the CCM/CCCM/PCM code family now includes five sets of codes, each set with a base code and an add-on code. The sets vary by the degree of complexity of care, who directly performs the services, and the time spent furnishing the services. The RUC-recommended values for work RVUs and direct PE inputs for these codes in CY 2022 were derived from a recent RUC specialty society survey.
CMS has finalized its proposal to create separate coding and payment for CPM services beginning January 1, 2023.
- HCPCS Code G3002: Chronic pain management and treatment, monthly bundle including, diagnosis; assessment and monitoring; administration of a validated pain rating scale or tool; the development, implementation, revision, and/or maintenance of a person-centered care plan that includes strengths, goals, clinical needs, and desired outcomes; overall treatment management; facilitation and coordination of any necessary behavioral health treatment; medication management; pain and health literacy counseling; any necessary chronic pain related crisis care; and ongoing communication and care coordination between relevant practitioners furnishing care, e.g. physical therapy and occupational therapy, and community-based care, as appropriate. Required initial face-to-face visit at least 30 minutes provided by a physician or other qualified health professional; first 30 minutes personally provided by physician or other qualified health care professional, per calendar month. (When using G3002, 30 minutes must be met or exceeded.)
- HCPCS code G3003: Each additional 15 minutes of chronic pain management and treatment by a physician or other qualified health care professional, per calendar month. (List separately in addition to code for G3002. When using G3003, 15 minutes must be met or exceeded.)
Revisions to “Incident To” Physicians’ Services Regulation for Behavioral Health Services
In the CY 2014 PFS final rule, CMS created an exception to its “incident to” regulation under which “incident to” services generally must be furnished under direct supervision, to allow general, rather than direct, supervision when chronic care management services are furnished incident to the billing physician’s or NPP’s services outside of the practice’s normal business hours by clinical staff. In the CY2017 PFS final rule, CMS also revised regulations to allow general, rather than direct, level of supervision for designated care management services, and established that it would designate care management services through notice and comment rulemaking.
CMS noted in the proposed rule that currently there is no separate benefit category under the statute that recognizes the professional services of licensed professional counselors (LPCs) and Licensed Marriage and Family Therapists (LMFTs). Therefore, payment for the services of LPCs and LMFTs can only be made under the PFS indirectly when an LPC or LMFT performs services as auxiliary personnel incident to, the services, and under the direct supervision, of the billing physician or other practitioner.
Given CMS’ goal in the 2022 CMS Behavioral Health Strategy to improve access to and quality of mental health care services, CMS finalizes several regulatory changes to make greater use of the services of LPCs and LMFTs. CMS notes that it does not have authority to create a statutory benefit category for practitioner types, but it finalizes its proposal to amend the direct supervision requirement under the “incident to” regulation to allow behavioral health services to be furnished under the general supervision of a physician or NPP when these services or supplies are provided by auxiliary personnel incident to the services of a physician or NPP.
CMS further clarifies that any service furnished primarily for the diagnosis and treatment of a mental health or SUD can be furnished by auxiliary personnel under the general supervision of a physician or NPP who is authorized to furnish and bill for the services provided incident to their own professional services.
CMS further plans to address payment for new codes that describe caregiver behavioral management training in the CY 2024 PFS.
New Coding and Payment for General Behavioral Health Integration (BHI) billed by Clinical Psychologists (CPs) and Clinical Social Workers (CSWs)
In the CY2017 and CY2018 PFS final rules, CMS established codes and payment for monthly services furnished using the Psychiatric Collaborative Care Model (CoCM), an evidence-based approach to behavioral health integration that enhances “usual” primary care by adding care management support and regular psychiatric inter-specialty consultation, and for services furnished using other models of BHI in the primary care setting.
In those rules, CMS additionally sought comment on the circumstances under which this model of care is happening and whether additional coding would be needed to accurately describe and value other models of care. CMS received feedback that initiating visit services for BHI should include in-depth psychological evaluations delivered by a CP, and that CMS should consider allowing professionals who were not eligible to report the approved initiating visit codes to Medicare to serve as a primary hub for BHI services.
CMS is now finalizing a proposal to create a new G code describing General BHI performed by CPs or CSWs to account for monthly care integration where the mental health services furnished by a CP or CSW are serving as the focal point of care integration. The finalized new code is :
- G0323 (Care management services for behavioral health conditions, at least 20 minutes of clinical psychologist or clinical social worker time, per calendar month, with the following required elements: initial assessment or follow-up monitoring, including the use of applicable validated rating scales; behavioral health care planning in relation to behavioral/psychiatric health problems, including revision for patients who are not progressing or whose status changes; facilitating and coordinating treatment such as psychotherapy, coordination with and/or referral to physicians and practitioners who are authorized by Medicare law to prescribe medications and furnish E/M services, counseling and/or psychiatric consultation; and continuity of care with a designated member of the care team.)
CMS has finalized its proposal to value this service under the proposed HCPCS code G0323 based on a direct crosswalk to the work values and direct PE inputs for CPT code 99484 (Care management services for behavioral health conditions, at least 20 minutes of clinical staff time, directed by a physician or other qualified health care professional, per calendar month, with the following required elements: initial assessment or follow-up monitoring, including the use of applicable validated rating scales; behavioral health care planning in relation to behavioral/psychiatric health problems, including revision for patients who are not progressing or whose status changes; facilitating and coordinating treatment such as psychotherapy, pharmacotherapy, counseling and/or psychiatric consultation; and continuity of care with a designated member of the care team), because the services described by GBHI1 closely mirror those described by CPT code 99484.
Modifications Related to Medicare Coverage for Opioid Use Disorder (OUD) Treatment Services Furnished by Opioid Treatment Programs (OTPs)
Section 2005 of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act established a new Medicare Part B benefit category for OUD treatment services furnished by OTPs during an episode of care beginning on or after January 1, 2020. CMS implemented Medicare coverage and provider enrollment requirements and established a methodology for determining the bundled payments for episodes of care for the treatment of OUD furnished by OTPs, among other related policies, in the CY2020 PFS final rule. CMS subsequently adopted new add-on codes and payment, and made certain policy changes, in the CY2021 and CY2022 final rules.
CMS has now finalized several additional updates to payment and policies regarding OUD treatment services furnished by OTPs.
- Methadone Pricing – CMS has finalized its revised methodology for pricing the drug component of the methadone weekly bundle and the add-on code for take-home supplies of methadone. CMS will base the payment amount for the drug component of HCPCS codes G2067 and G2078 for CY 2023 and subsequent years on the payment amount for methadone in CY 2021 and update this amount annually to account for inflation using the PPI for Pharmaceuticals for Human Use (Prescription).
- Proposed Changes to the Rate for Individual Therapy in the Bundled Rate – CMS has finalized its proposal to modify the payment rate for the non-drug component of the bundled payments for episodes of care to base the rate for individual therapy on a crosswalk code describing a 45-minute session, rather than the current crosswalk to a code describing a 30-minute session.
- Mobile Components Operated by OTPs – CMS clarifies that OTPs can bill Medicare for medically reasonable and necessary services furnished via mobile units in accordance with SAMHSA and DEA guidance. CMS finalizes its proposal that locality adjustments for services furnished via mobile units would be applied as if the service were furnished at the physical location of the OTP registered with DEA and certified by SAMHSA.
- Flexibilities for OTPs to Use Telecommunications for Initiation of Treatment with Buprenorphine – CMS has finalized its proposal to allow the OTP intake add-on code to be furnished via two-way audio-video communications technology when billed for the initiation of treatment with buprenorphine, to the extent that the use of audio-video telecommunications technology to initiate treatment with buprenorphine is authorized by DEA and SAMHSA at the time the service is furnished. CMS also finalizes its proposal to permit the use of audio-only communication technology to initiate treatment with buprenorphine in cases where audio-video technology is not available to the beneficiary.
Comment Solicitation on Intensive Outpatient Mental Health Treatment, including Substance Use Disorder (SUD) Treatment, Furnished by Intensive Outpatient Programs (IOPs)
CMS noted in the proposed rule that there are a range of services described by existing coding under the PFS that can be billed for treatment of mental health conditions, including SUDs, such as individual, group, and family psychotherapy. Over the past several years, CMS has increased the coding and payment mechanisms for substance use treatment services paid under the PFS.
CMS requested feedback on whether the current coding and payment mechanisms under the PFS adequately account for intensive outpatient services that are part of a continuum of care in the treatment, among other information.
CMS thanks commenters for their feedback and may consider the comments in future rulemaking.
Comment Solicitation on Payment for Behavioral Health Services under the PFS
CMS solicited comment on how it can best ensure beneficiary access to behavioral health services, including any potential adjustments to the PFS rate-setting methodology, for example, any adjustments to systematically address the impact on behavioral health services paid under the PFS.
CMS noted that it appreciates the feedback received and may consider the comments in future rulemaking.
Medicare Telehealth Analysis
Share This Study!
Fall 2022
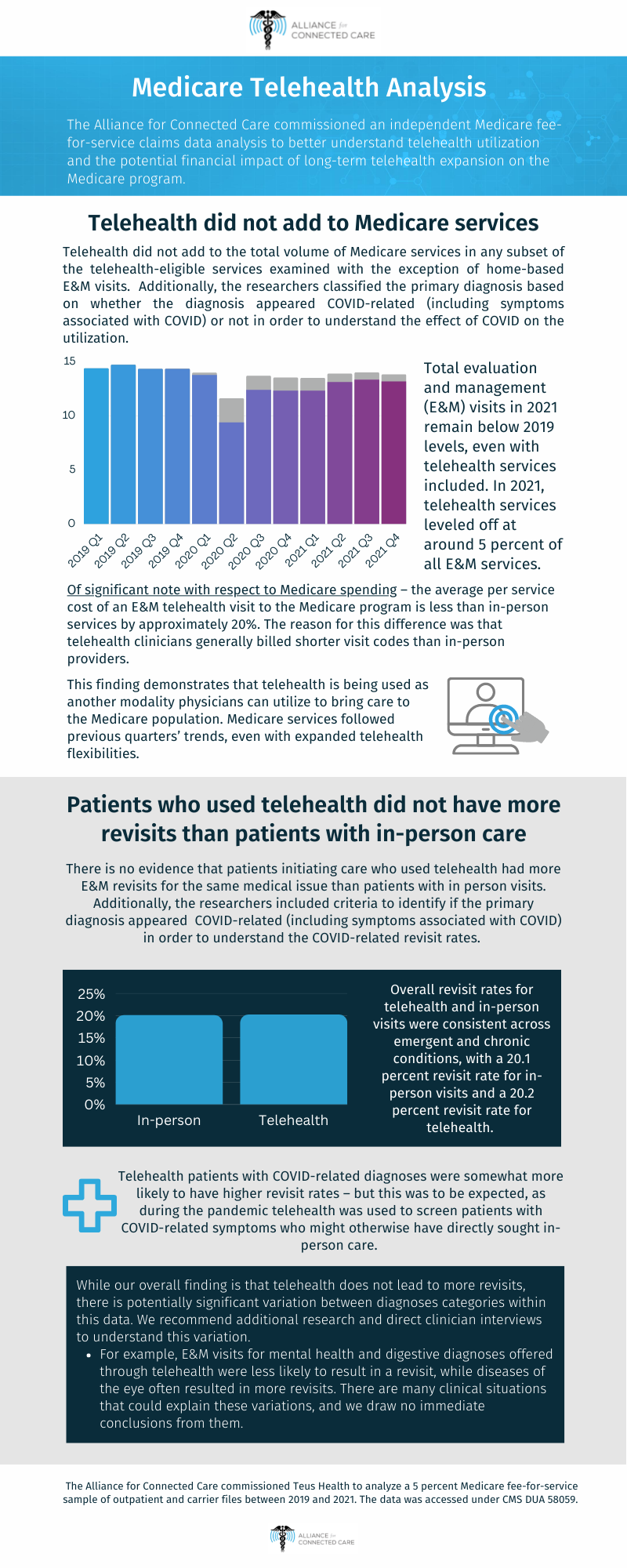
The Alliance for Connected Care commissioned an independent Medicare claims data analysis to better understand telehealth utilization and the potential financial impact of long-term telehealth expansion on the Medicare program. As expected, the findings of this analysis align with the individual experiences and data collected by Alliance for Connected Care members.
“It’s hard to break conventional wisdom in Washington. We finally have comprehensive telehealth utilization data in Medicare that should rectify the misconception that telehealth is somehow uniquely subject to over-use.” – Krista Drobac, Alliance for Connected Care
The research project, executed by Teus Health, fully analyzed Medicare fee-for-service claims data[1] across three full years – 2019, 2020, and 2021 – to answer and further explore the following crucial questions:
- Is telehealth adding to the total volume of Medicare services or replacing in-person services?
- Compared to patients who had an initial in-person visit, did patients who had a telehealth visit have more follow-up visits?
We expect this research to be useful to the Congressional Budget Office, MedPAC, and other entities which have expressed concerns that telehealth legislation may lead to additional costs for the Medicare program.
Finding 1: There is no evidence that telehealth is adding to the total volume of Medicare services.
The analysis examined the utilization of services to determine better understand if telehealth is adding to the total volume of Medicare services or replacing in-person services. Additionally, the researchers classified the primary diagnosis based on whether the diagnosis appeared Covid-related (including symptoms associated with Covid) or not in order to understand the effect of COVID on the utilization.
- Total evaluation and management (E&M) visits in 2021 remain below 2019 levels, even with telehealth services included. In 2021, telehealth services leveled off at around 5 percent of all E&M services.
[1] Source: Medicare 5% sample, outpatient and carrier files, 2019-2021, accessed under CMS DUA 58059.
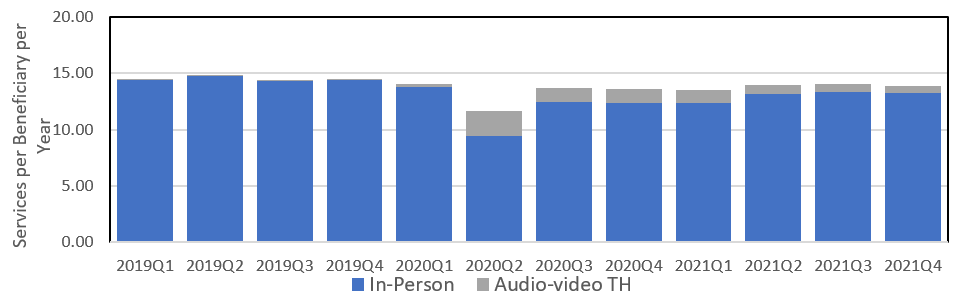
- Telehealth did not add to the total volume of Medicare services in any subset of the telehealth-eligible services examined with the exception of home-based E&M visits. Telehealth continues to represent a larger percentage of home visits than overall E&M visits.
- Of significant note with respect to Medicare spending – the average per service cost of an E&M telehealth visit to the Medicare program is less than in-person services by approximately 20%. The reason for this difference was that telehealth clinicians generally billed shorter visit codes than in-person providers.
- Provider types most heavily relying on telehealth included all mental health and substance use disorder providers, primary care clinicians, as well as endocrinologists, pain management, anesthesiology, and sleep medicine specialties.
- This finding demonstrates that telehealth is being used as another modality physicians can utilize to bring care to the Medicare population. Medicare services followed previous quarters’ trends, even with expanded telehealth flexibilities.
Finding 2: There is no evidence that patients initiating care who used telehealth had more E&M revisits for the same medical issue than patients with in-person visits.
The analysis examined revisit rates to answer whether patients who had a telehealth E&M visit had more follow-up visits than patients who had an initial in-person visit. Additionally, the researchers included criteria to identify if the primary diagnosis appeared COVID-related (including symptoms associated with COVID) in order to understand the COVID-related revisit rates.
-
- Overall revisit rates for telehealth and in-person visits were consistent across emergent and chronic conditions, with a 20.1 percent revisit rate for in-person visits and a 20.2 percent revisit rate for telehealth.
- Telehealth patients with COVID-related diagnoses were somewhat more likely to have higher revisit rates – but this was to be expected, as during the pandemic telehealth was used to screen patients with COVID-related symptoms who might otherwise have directly sought in-person care.
- While our overall finding is that telehealth does not lead to more revisits, there is potentially significant variation between diagnoses categories within this data. We recommend additional research and direct clinician interviews to understand this variation.
- For example, E&M visits for mental health and digestive diagnoses offered through telehealth were less likely to result in a revisit, while diseases of the eye often resulted in more revisits. There are many clinical situations that could explain these variations, and we draw no immediate conclusions from them.
See the analysis below or here.
 Loading...
Loading...
Telemedicine management of type 2 diabetes mellitus in obese and overweight young and middle-aged patients during COVID-19 outbreak: A single-center, prospective, randomized control study
PLoS One: Telemedicine management of type 2 diabetes mellitus in obese and overweight young and middle-aged patients during COVID-19 outbreak: A single-center, prospective, randomized control study
Objective: The coronavirus disease-2019 (COVID-19) pandemic severely affected the disease management of patients with chronic illnesses such as type 2 diabetes mellitus (T2DM). This study aimed to assess the effect of telemedicine management of diabetes in obese and overweight young and middle-aged patients with T2DM during the COVID-19 pandemic.
Methods: A single-center randomized control study was conducted in 120 obese or overweight (body mass index [BMI] ≥ 24 kg/m2) young and middle-aged patients (aged 18-55 years) with T2DM. Patients were randomly assigned to the intervention (telemedicine) or control (conventional outpatient clinic appointment) group. After baseline assessment, they were home isolated for 21 days, received diet and exercise guidance, underwent glucose monitoring, and followed up for 6 months. Glucose monitoring and Self-Rating Depression Scale (SDS) scores were evaluated at 22 days and at the end of 3 and 6 months.
Results: Ninety-nine patients completed the 6-month follow-up (intervention group: n = 52; control group: n = 47). On day 22, the fasting blood glucose (FBG) level of the intervention group was lower than that of the control group (p < 0.05), and the control group’s SDS increased significantly compared with the baseline value (p < 0.05). At the end of 3 months, glycated hemoglobin (HbA1c) and FBG levels in the intervention group decreased significantly compared with those in the control group (p < 0.01). At the end of 6 months, the intervention group showed a significant decrease in postprandial blood glucose, triglyceride, and low-density lipoprotein cholesterol levels as well as waist-to-hip ratio compared with the control group (p < 0.05); moreover, the intervention group showed lower SDS scores than the baseline value (p < 0.05). Further, the intervention group showed a significant reduction in BMI compared with the control group at the end of 3 and 6 months (p < 0.01).
Conclusion: Telemedicine is a beneficial strategy for achieving remotely supervised blood glucose regulation, weight loss, and depression relief in patients with T2DM.
Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis
Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis
Background: Telemedicine has been increasingly integrated into chronic disease management through remote patient monitoring and consultation, particularly during the COVID-19 pandemic. We did a systematic review and meta-analysis of studies reporting effectiveness of telemedicine interventions for the management of patients with cardiovascular conditions.
Methods: In this systematic review and meta-analysis, we searched PubMed, Scopus, and Cochrane Library from database inception to Jan 18, 2021. We included randomised controlled trials and observational or cohort studies that evaluated the effects of a telemedicine intervention on cardiovascular outcomes for people either at risk (primary prevention) of cardiovascular disease or with established (secondary prevention) cardiovascular disease, and, for the meta-analysis, we included studies that evaluated the effects of a telemedicine intervention on cardiovascular outcomes and risk factors. We excluded studies if there was no clear telemedicine intervention described or if cardiovascular or risk factor outcomes were not clearly reported in relation to the intervention. Two reviewers independently assessed and extracted data from trials and observational and cohort studies using a standardised template. Our primary outcome was cardiovascular-related mortality. We evaluated study quality using Cochrane risk-of-bias and Newcastle-Ottawa scales. The systematic review and the meta-analysis protocol was registered with PROSPERO (CRD42021221010) and the Malaysian National Medical Research Register (NMRR-20-2471-57236).
Findings: 72 studies, including 127 869 participants, met eligibility criteria, with 34 studies included in meta-analysis (n=13 269 with 6620 [50%] receiving telemedicine). Combined remote monitoring and consultation for patients with heart failure was associated with a reduced risk of cardiovascular-related mortality (risk ratio [RR] 0·83 [95% CI 0·70 to 0·99]; p=0·036) and hospitalisation for a cardiovascular cause (0·71 [0·58 to 0·87]; p=0·0002), mostly in studies with short-term follow-up. There was no effect of telemedicine on all-cause hospitalisation (1·02 [0·94 to 1·10]; p=0·71) or mortality (0·90 [0·77 to 1·06]; p=0·23) in these groups, and no benefits were observed with remote consultation in isolation. Small reductions were observed for systolic blood pressure (mean difference -3·59 [95% CI -5·35 to -1·83] mm Hg; p<0·0001) by remote monitoring and consultation in secondary prevention populations. Small reductions were also observed in body-mass index (mean difference -0·38 [-0·66 to -0·11] kg/m2; p=0·0064) by remote consultation in primary prevention settings.
Interpretation: Telemedicine including both remote disease monitoring and consultation might reduce short-term cardiovascular-related hospitalisation and mortality risk among patients with heart failure. Future research should evaluate the sustained effects of telemedicine interventions.